Search
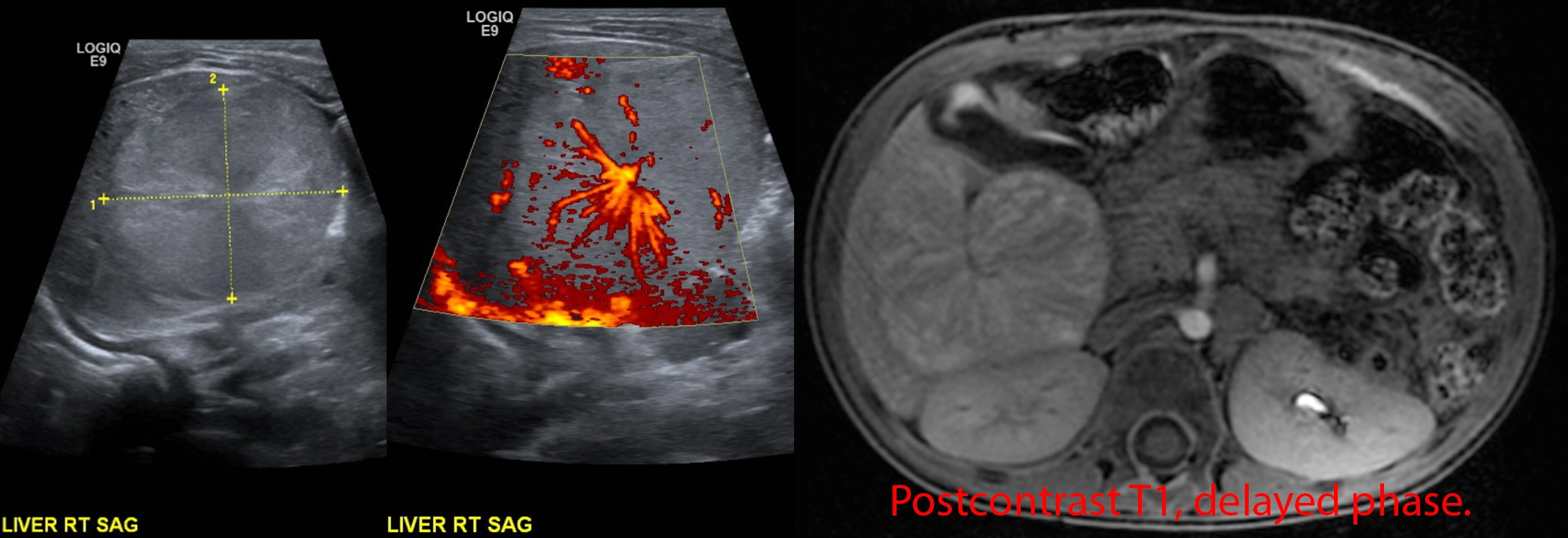
Optic neuritis.
5 year old patient with 1 week of right eye blurry vision, then several days of right eye pain. Physical exam notable for right papilledema and progressively worsening vision.
MRI postcontrast through the orbits shows an enlarged, hyperenhancing right optic nerve (red arrow) compared to the normal left side (green arrow), compatible with optic neuritis.
A lumbar puncture was performed: no oligoclonal bands, no aquaporin 4 IgG, positive anti-MOG. The patient was treated with prednisone with return to normal vision a few months later.
Final diagnosis: optic neuritis from myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD).
Electric shooting pains in the left face.

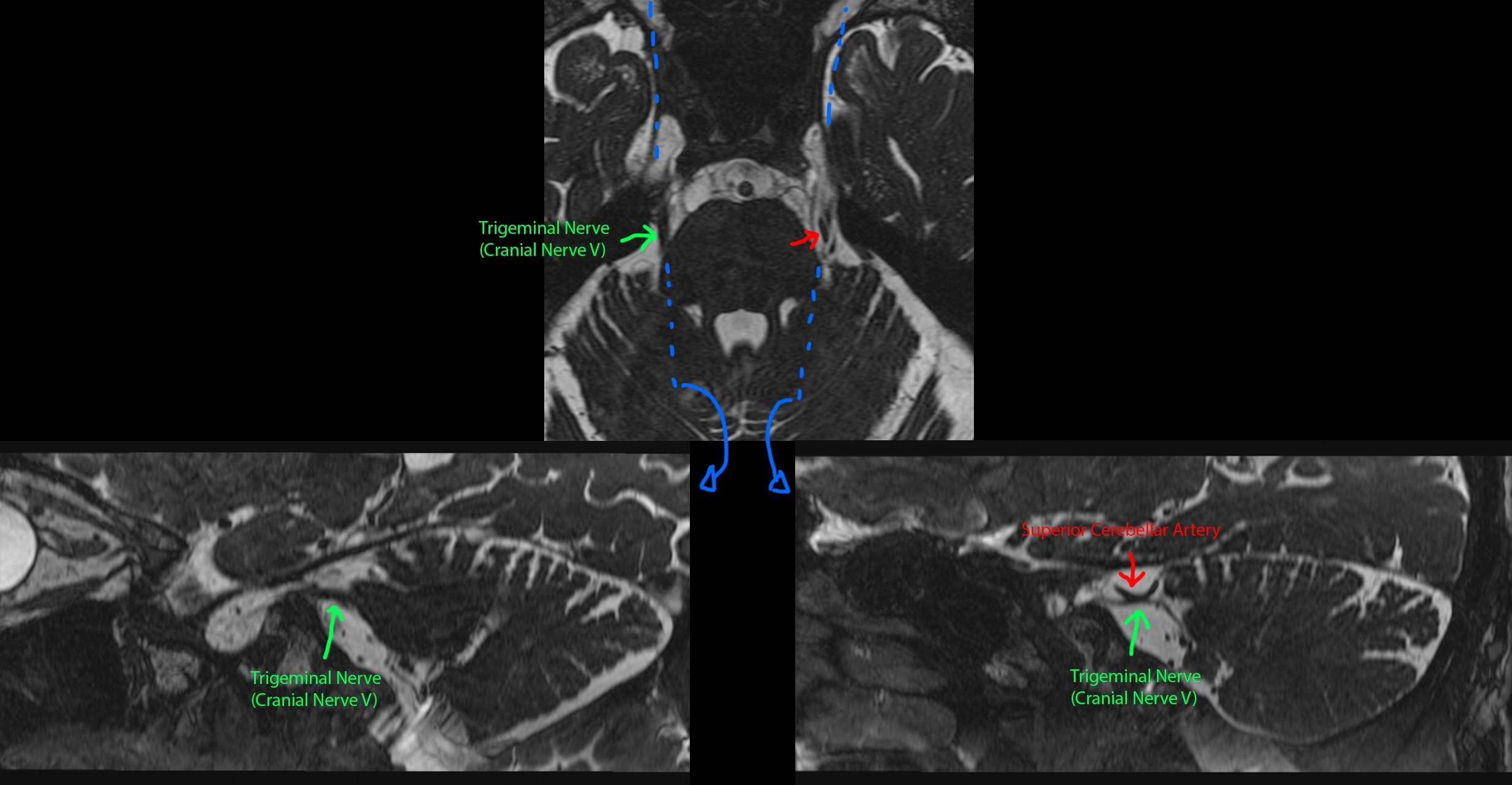
This patient had episodic electric/shooting/radiating pain of the left face. An MRI was done.
[Top]: Axial heavily T2-weighted image (bright = CSF, dark = not CSF) at the level of trigeminal nerve (cranial nerve V / CN5), shows a normal right CN5 (green). The left CN5 seems to be splayed out by another tubular structure (red), which is the superior cerebellar artery (SCA).
[Bottom Left]: Sagittal reconstruction of the normal right CN5 (along the blue line).
[Bottom Right]: Sagittal reconstruction of the left CN5 shows the left SCA contacting the left CN5. The close proximity of the left SCA and its arterial pulsations likely irritate the cranial nerve, which is the primary sensory nerve of the face, causing trigeminal neuralgia.
Chiari 1 malformation.

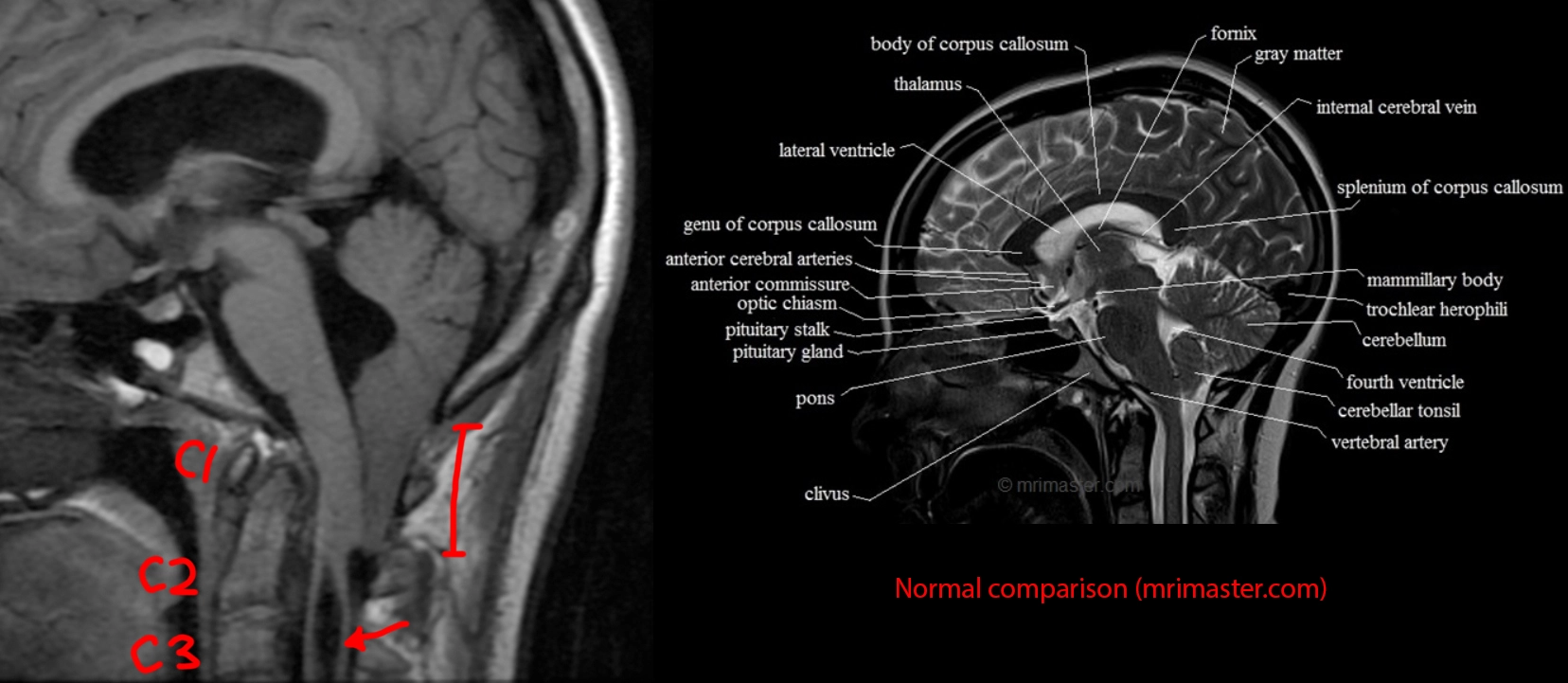
[LEFT]: This patient had one of the longer cerebellar tonsillar herniations I've seen. The tonsil is peg-like in shape and extends quite far below the foramen magnum to the level of the C2 posterior arch. As a result, there is crowding at the foramen magnum that is enough to impede CSF flow, resulting in hydrocephalus with dilated ventricles. Partly seen in the cervical cord from C2 and below is a syrinx, an associated finding. Chiari I is thought to be due to not enough space provided for the cerebellum by the calvarium or skull base shape, causing it to herniate into the spinal canal and cause trouble.
[RIGHT]: A comparison normal from online for you to compare the cerebellar tonsils.
Molar tooth deformity in Joubert syndrome.
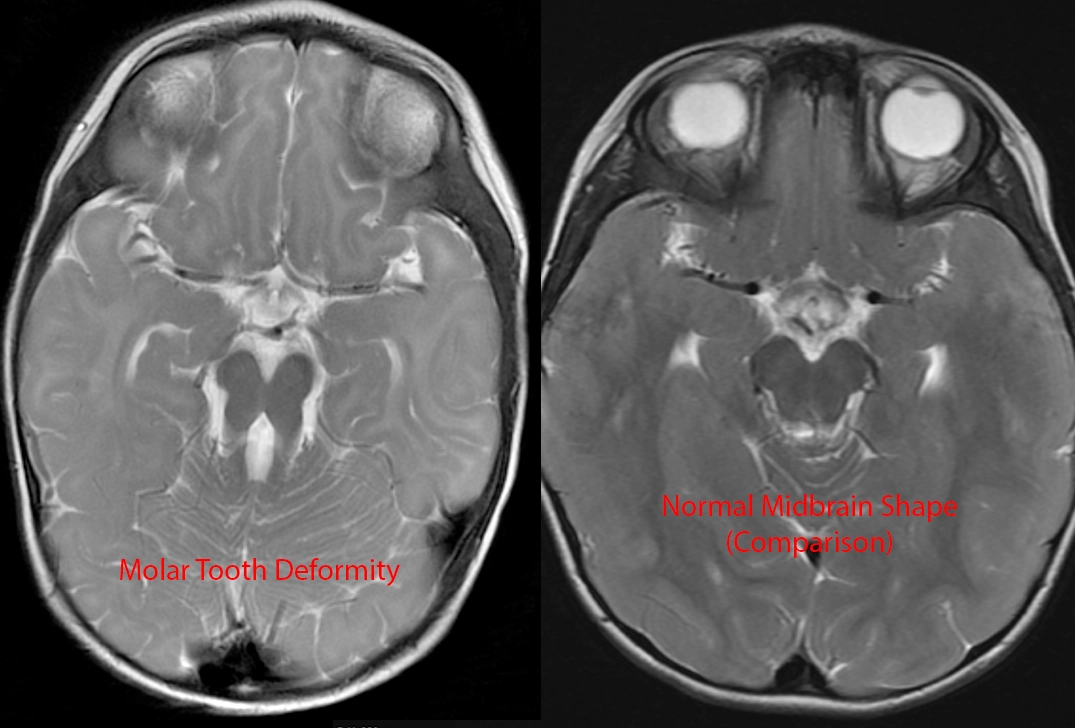
[LEFT]: The midbrain has a deep interpeduncular cistern, and the superior cerebellar peduncles are very prominent and elongated, making the brainstem at this level look like a molar tooth. This is a classic finding in Joubert syndrome.
[RIGHT]: A comparison "normal" midbrain. However, this patient's brain is not normal at all. Can you find the abnormalities?
Answer
Compare the left and right temporal lobes in [RIGHT] to the [LEFT] image. Look at how many more gyri and sulci there are in the [LEFT] image. The [RIGHT] patient has a diffuse pachygyria (abnormally reduced brain gyrations). Both Joubert syndrome and pachygyria arise from failure of neurons to migrate, although the genes involved and underlying mechanism are different between the two. (NB: Pachygyria is just a descriptive term for less than normal number of gyri, which can be from a large number of causes mostly having to do with abnormal neuron migration.)
Painful left shoulder.

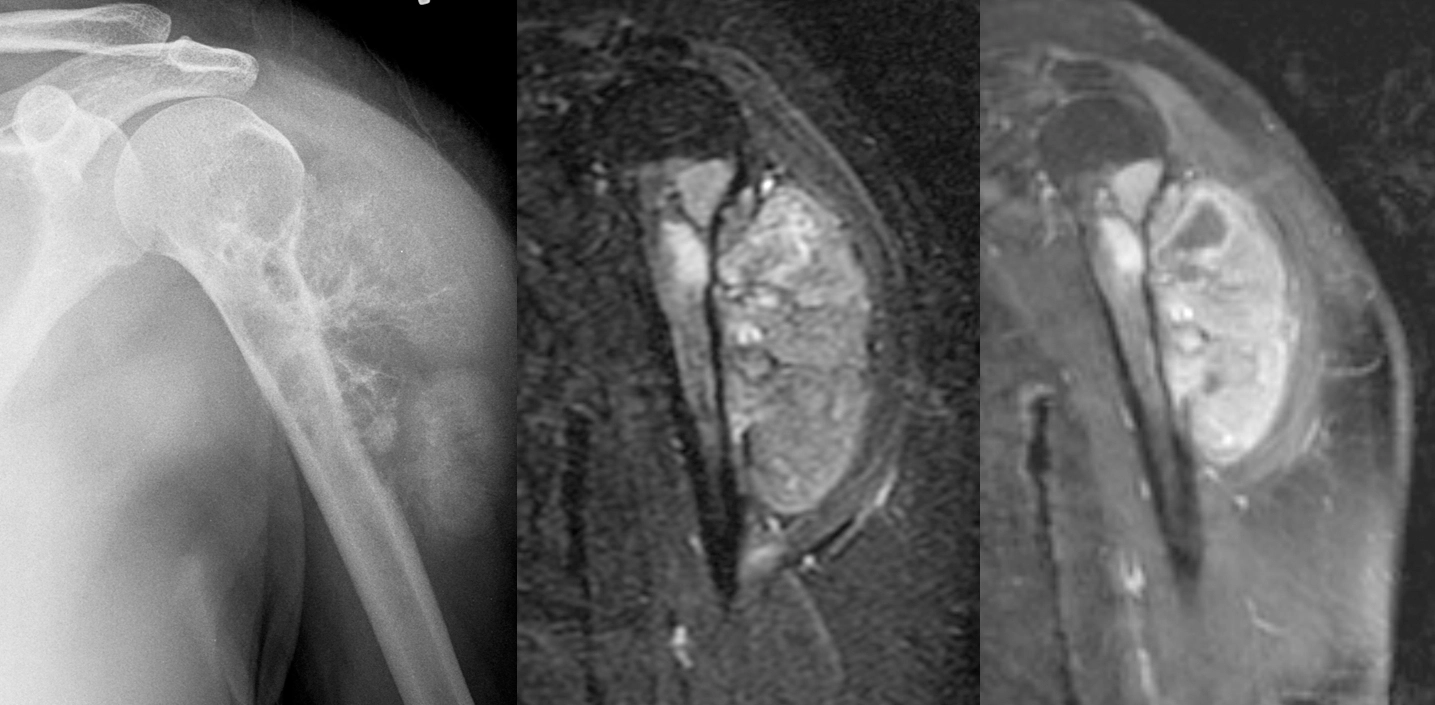
Female in her 30s with painful left shoulder.
[Left]: X-ray shows a mass arising from the left proximal humerus and extending into the adjacent shoulder soft tissues with really aggressive periosteal reaction ("hair on end"). The proximal humerus itself is also heterogeneous with lucent areas. The lateral surface of the upper humerus shows "saucerization," where the cortex is thinned out and looks like a saucer seen on edge.
[Middle]: MRI IR sequence shows a hyperintense bony mass with large soft tissue component.
[Right]: MRI postcontrast T1 IDEAL shows that the mass is enhancing.
This turned out to be high-grade surface osteosarcoma.
Butterfly glioma.

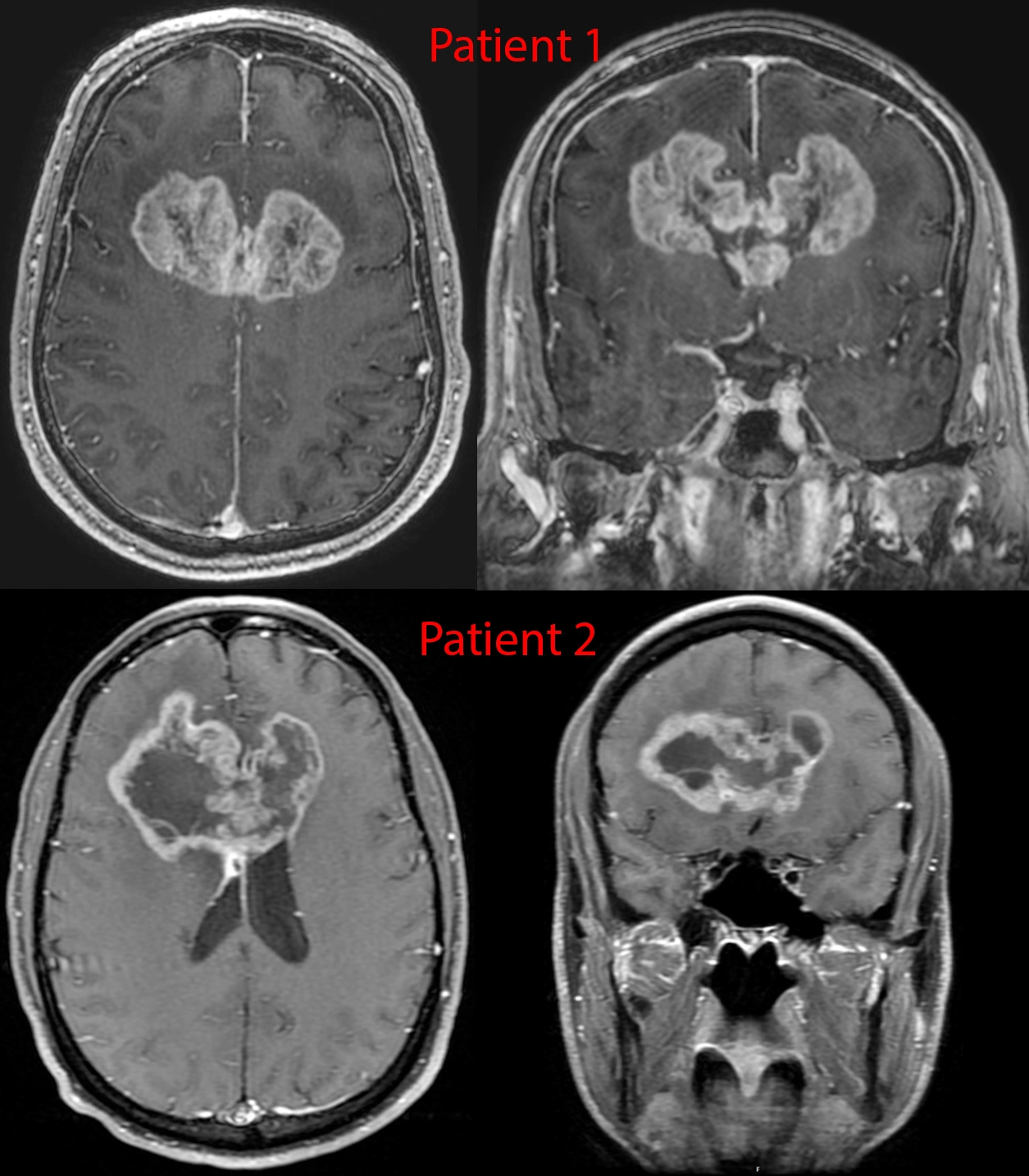
Postcontrast imaging of 2 patients with glioblastoma. These tumors are notorious for spreading along the white matter tracts - in this case the transverse fibers of the corpus callosum, given them a classic "butterfly" appearance.
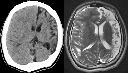
Hemimegaencephaly.
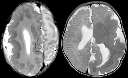
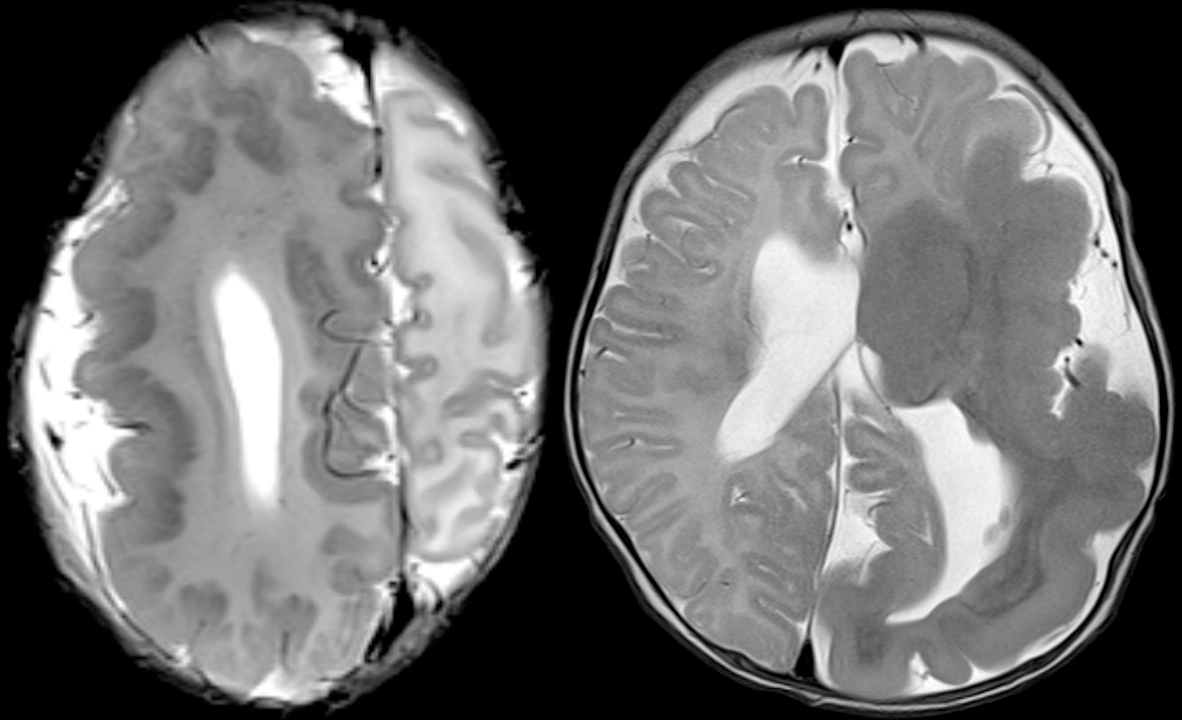
Two different patients with genetic disorders resulting in overgrowth of the brain.
These represent mutations in cell cycle and cell metabolism genes that lead to larger cells and/or more cells. These types of disorders tend to have mosaicism of some form, which is to say some cells have the mutation active while others don't. The distribution of these cells can be very geographic/regional - in these two cases, one hemisphere of the brain is involved.
Compare this against a previous case with hemispheric atrophy.
Unusual complication of cocaine abuse.
Patient was a young adult working in finance at a major tech company found to be mute and diaphoretic.
Physical exam notable for fever, tachycardiac, hypertension, awake but not following commands, aphasic, and with hyperreflexia and muscle ridigity. CK peaked to 11,344.
MRI shows multiple ovoid to splotchy confluent lesions in the white matter with diffusion restriction. Lesions also enhanced with hyperperfusion (not shown).
Urine drug test positive for cocaine. Infectious work-up was negative. Steroids were started with good recovery.
Patient denied knowingly taking cocaine but did say weekly use of what they thought was MDMA with friends...
Final diagnosis: Levamisole-induced leukoencephalopathy. Levamisole is an antiparasite medication that is no longer used in the US but still in some other countries. It is a common cutting agent in cocaine. It's neurotoxic effects primarily come from causing demyelination.
House, MD, pilot episode.

I remember this episode quite well because it happened around the time I decided to get into the medical field. In the episode, a young teacher had a first-time seizure while in the middle of teaching. House and team attempted to get a brain MRI, but she got an allergic reaction from the IV contrast. Thereafter, some drama happens, and at some point, they break into her house, find out she's been eating raw pork (wtf?), and diagnose her with the tapeworm infection associated with eating raw pork, cysticercosis (and neurocysticercosis, since it also involved her brain). They took an x-ray of her leg to show all the parasites in the muscles, and then House scolds her for being stupid. I remember thinking that was such as crazy medical story.
The reality is - they could have just repeated the brain MRI minus the contrast part, and the radiologist would have been able to identify neurocysticercosis without issue. House would have complained to Cuddy that she really was wasting his time with these basic cases, and the episode would have lasted 15 minutes tops...
Anyhow, this is a 25 year old Hispanic from jail. Just like the House episode, he presented with first time seizure and headaches.
CT of the head [top] shows a cystic lesion in the left frontal lobe. If one pays attention, one can see a small dot (blue arrow) within the cyst representing the scolex of the tapeworm parasite. Just from the CT appearance, history of seizure, and risk factors of jail (the parasite thrives in areas of low sanitation) and Hispanic (the parasite is endemic to South America), neurocysticercosis is the top possibility. A differential diagnosis of cystic brain tumor is provided to complete the picture.
MR [middle and bottom] shows a cystic lesion again. After giving IV contrast [middle right], one can see the cyst has a thin wall of enhancement (teal arrows). On T2 [bottom left] and especially FLAIR [bottom right], one can see a rim of swollen brain (green arrows) from the inflammation going on around the parasite.
This was diagnosed as neurocysticercosis in the colloidal vesicular stage and antiparasite medication was started.
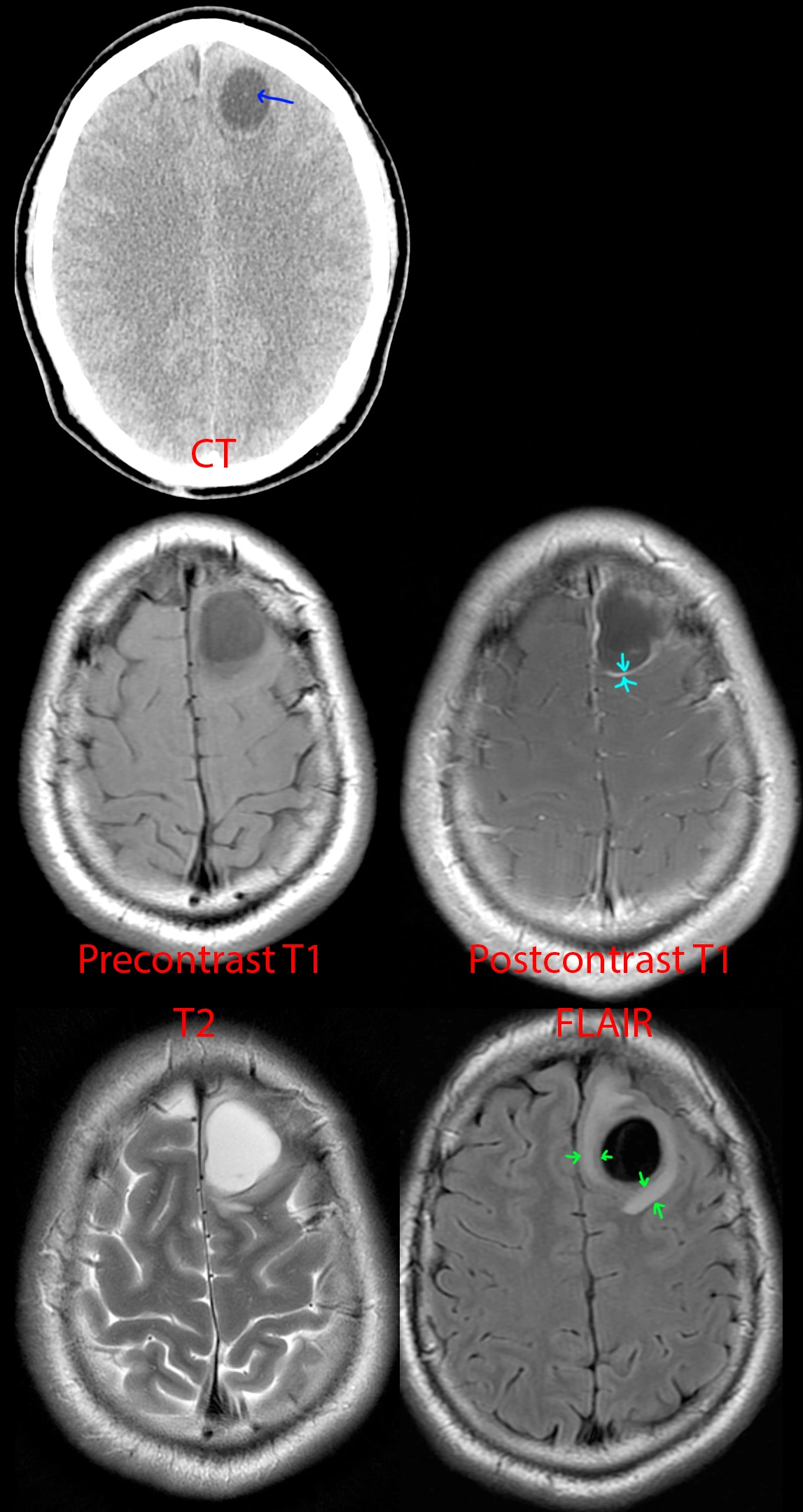
10 year old with insidious onset of right medial thigh pain.

[Top]: X-ray shows a lucent, bubbly, lesion of the distal femur at the metaphysis. On the frontal view [top right], there is breakage through the medial femoral cortex into the adjacent soft tissues, not a good sign.
[Bottom]: MRI shows a multicystic lesion filling the distal femur containing multiple locules, many with fluid-fluid, fluid-debris, and fluid-hemorrhage levels. The most common lesions with this striking appearance are aneurysmal bone cyst, giant cell tumor, or telangiectatic osteosarcoma. Unfortunately, there is clearly extension of the bone tumor beyond the bone (yellow arrows), which favors a more aggressive neoplasm from that differential diagnosis - this turned out to be telangiectatic osteosarcoma.
23 year old with head injury since age 2. Seizures and right hemiparesis since age 10.
[Left]: Head CT shows left hemispheric volume loss. The injury happened early enough that even the skull is smaller on that side.
[Right]: Brain MRI shows the severe left hemispheric atrophy. Some of the brain gyri have bulbous ends and a thin neck, resembling mushrooms, a shape called ulegyria and consequence of the brain atrophy. The left lateral ventricle is mildly enlarged due to the atrophied brain.
Conjoined twin, from prenatal to postnatal.


[Left]: Fetal MRI (FIESTA sequence) shows twins joined from their lower chest to the pelvis, but truly fused and sharing a single abnormal pelvic region. Not shown, but there are 3 lower limbs - one of the twins only had a single lower extremity.
[Right]: Postnatal small bowel follow-through (SBFT). It was unclear initially whether the twins shared a single rectum or had their own rectum. Therefore, contrast was administered via nasogastric tube for the twin with the suspected nonfunctional rectum, and serial imaging was performed until it passed into what turned out to be a separate, functional, but small rectum/anus.
I do not know too much about conjoined twins - not my area of expertise, but the general forms to consider are the side of fusion: ventral (front to front), lateral (side to side), dorsal (back to back), or caudal (tail end to tail end). Within these first 3, there are subtypes depending on how far up the fusion goes (head, chest, abdomen/pelvis); by definition, the caudal version obviously is only a lower body fusion. Once this is derived, an additional classification is the number of upper and lower limbs.
Nasal proboscis.

Not the best quality, but this is the only image I saved of this fetal MRI, with a random internet picture of what it would look like after birth.
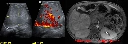
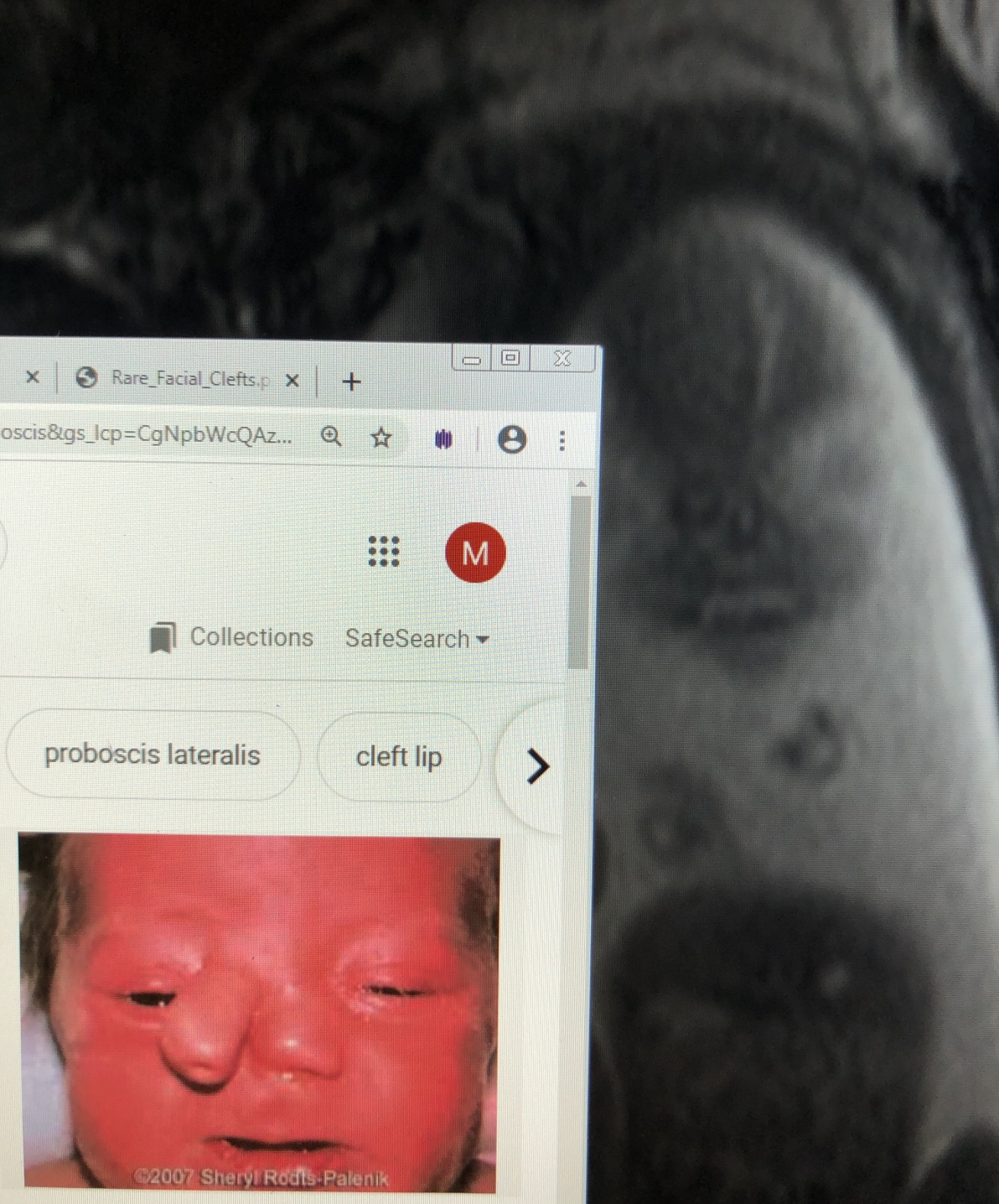
New shortness of breath on exertion with no past medical history.
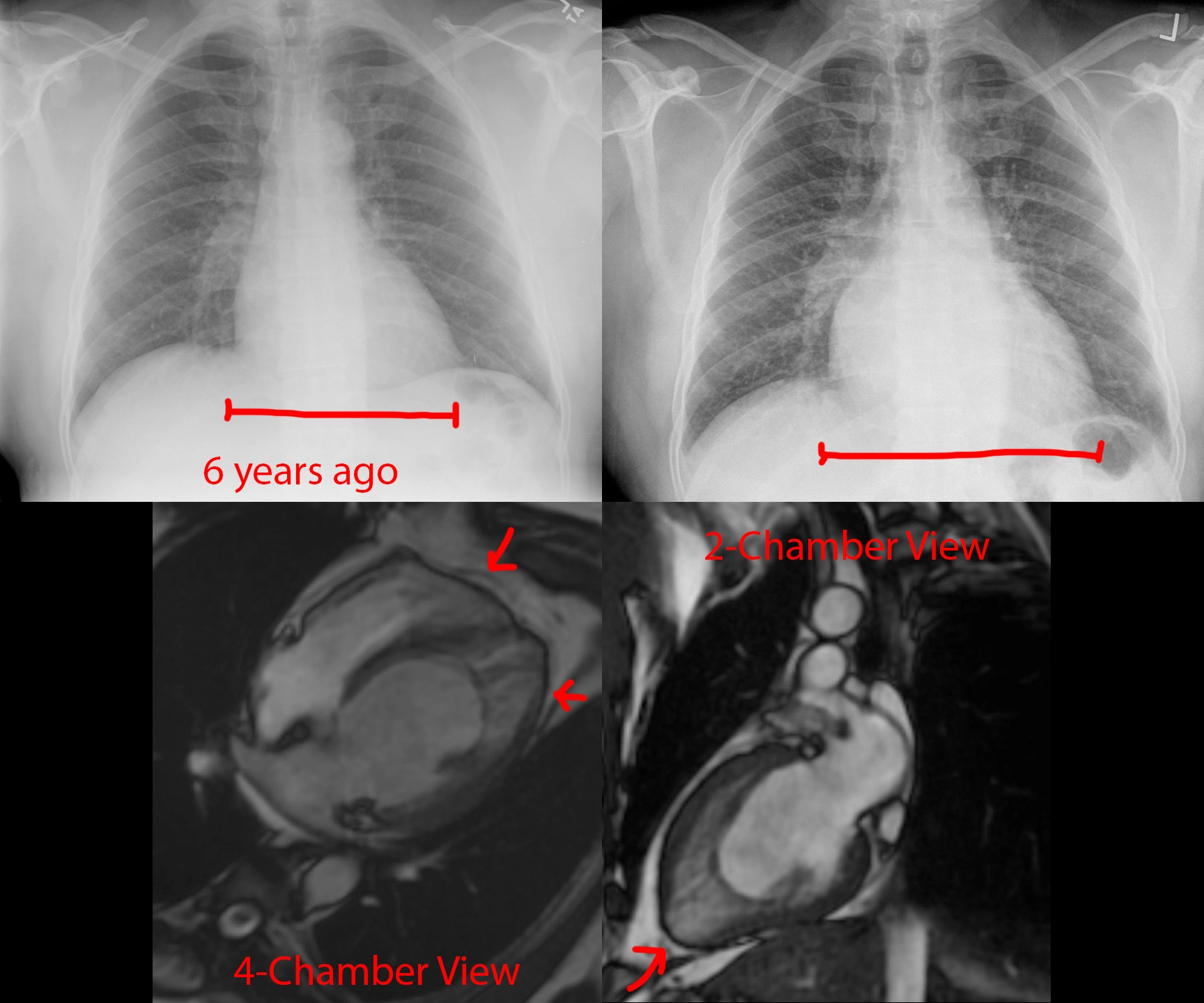
59 year old with no past medical history, now with new dyspnea on exertion.
Top: Chest radiographs show development of cardiomegaly since 6 years prior. The pulmonary vascular markings are also more prominent than before, suggesting pulmonary congestion.
Bottom: MRI Cine FIESTA sequences in the 4- and 2-chamber views at end-diastole. There are prominent trabeculations towards the cardiac apex at both the left and right ventricles. In particular, there is an outer layer of dense myocardium and a thicker inner layer of trabeculated myocardium.
Final Diagnosis: Cardiac noncompaction.
Comparison Case: Meth-Induced Cardiomyopathy.
Cardiac noncompaction is a genetic disorder leading to failure of the myocardium to form "compact" walls. It is extremely rare. The presentation depends on how bad the noncompaction is, so can be asymptomatic to heart failure, arrhythmias, and thromboembolism.
HIV-AIDS with tuberculosis with WORSENING symptoms after treatment started.
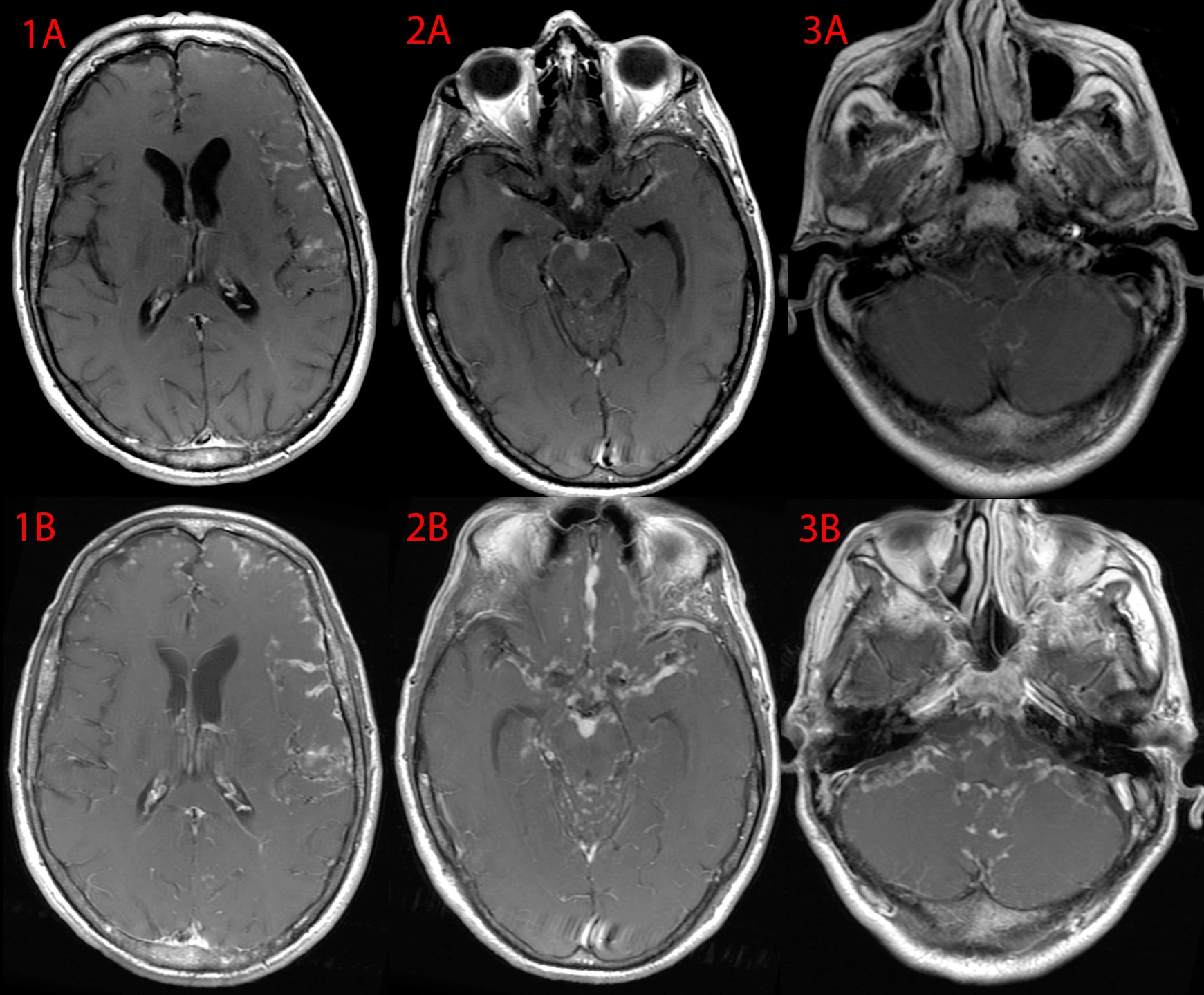
20 year old with HIV-AIDS and tuberculosis with intracranial involvement (TB meningitis), not on treatment for these things.
Appropriate treatment was started, including TB medications and anti-retrovirals for HIV. 2 weeks later, the patient had decreased levels of consciousness.
Top images [A] show the brain at 3 different levels on postcontrast MRI prior to treatment. Bottom images [B] show the follow-up MRI at the time of worsening neurologic status. There is a clear progression of nodular leptomeningeal enhancement throughout the brain.
Taking the above findings into context with the time of treatment, this was felt to be consistent with immune reconstitution inflammatory syndrome, an exaggerated immune response to a co-infection (TB) when a person's immune deficiency (HIV-AIDS) is corrected. High-dose steroids were started with significant improvement. One month later, a steroid taper was attempted, but the TB-IRIS relapsed. Ultimately, it took a year of slow taper to get the patient off the steroids while continuing to treat the HIV and TB.
Progressive cognitive decline.
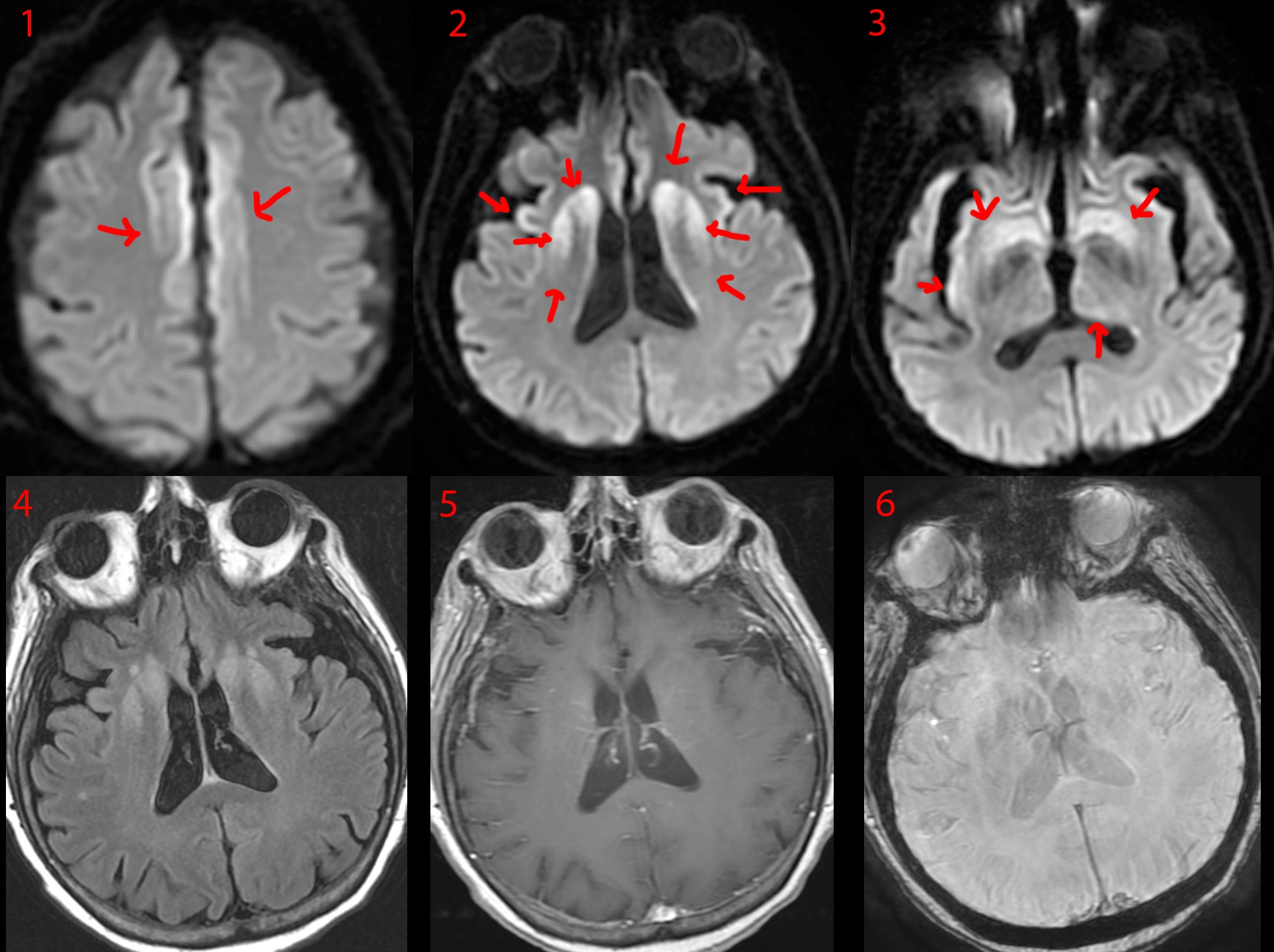
66 year old with progressive cognitive and neurological decline, becoming catatonic within 2 months.
MRI DWI [1, 2, 3] shows cortical ribboning (cortex diffusion restriction [1]), and diffusion restriction in the deep gray nuclei and insula [2, 3] in a symmetric fashion.
MRI FLAIR [4] shows abnormal bright signal at the sites of diffusion restriction.
MRI postcontrast T1 [5] and SWI [6] are normal.
Based on the above findings, there was a strong suspicion this was something bad. A lumbar puncture was performed under appropriate infection control guidelines. Results showed positive CSF results for 14-3-3, T-tau protein, and RT-QuIC. The patient had already been discharged to a nursing facility when these results came back, so the nursing facility was notified as well as the public health department. The patient was placed on comfort care.
Final diagnosis: sporadic Creutzfeldt-Jakob disease (CJD).
Atretic parietal cephalocele.

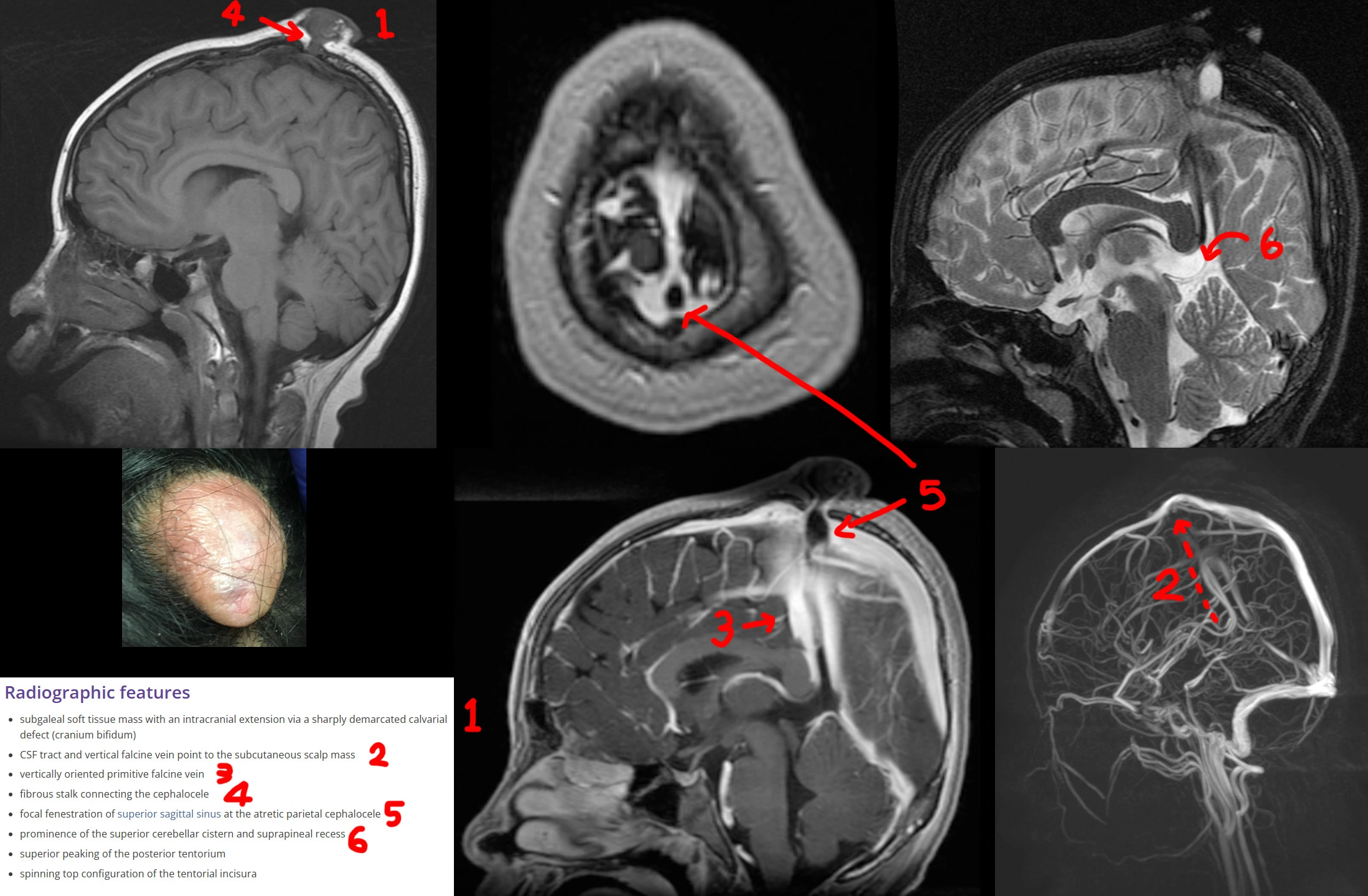
Photo: 8 year old with a mass at the top of his head since birth.
Top left: Sagittal T1 shows a pedunculated mass protruding through the midline calvarium.
Top & bottom mid: Sagittal postcontrast T1 SPGR shows the relation of the hairpin-shaped vessel and the superior sagittal sinus to the scalp mass. There is a fenestration (hole) in the superior sagittal sinus through which the fibrous stalk courses.
Top right: Sagittal T2 shows a hairpin-shaped vessel directed towards the lesion.
Bottom right: 3D MR venogram shows the hairpin-shaped vessel pointing towards the lesion.
Atretic parietal cephalocele is a congenital abnormal herniation of the brain covering +/- brain through a midline defect of the parietal bones. It is atretic because this herniation then atrophies until only a fibrous stalk connects it to the rest of the intracranial compartment. It is associated with a persistent falcine sinus, an embryonic vertical positioning of the straight sinus.
Gnathic (jaw) osteosarcoma.

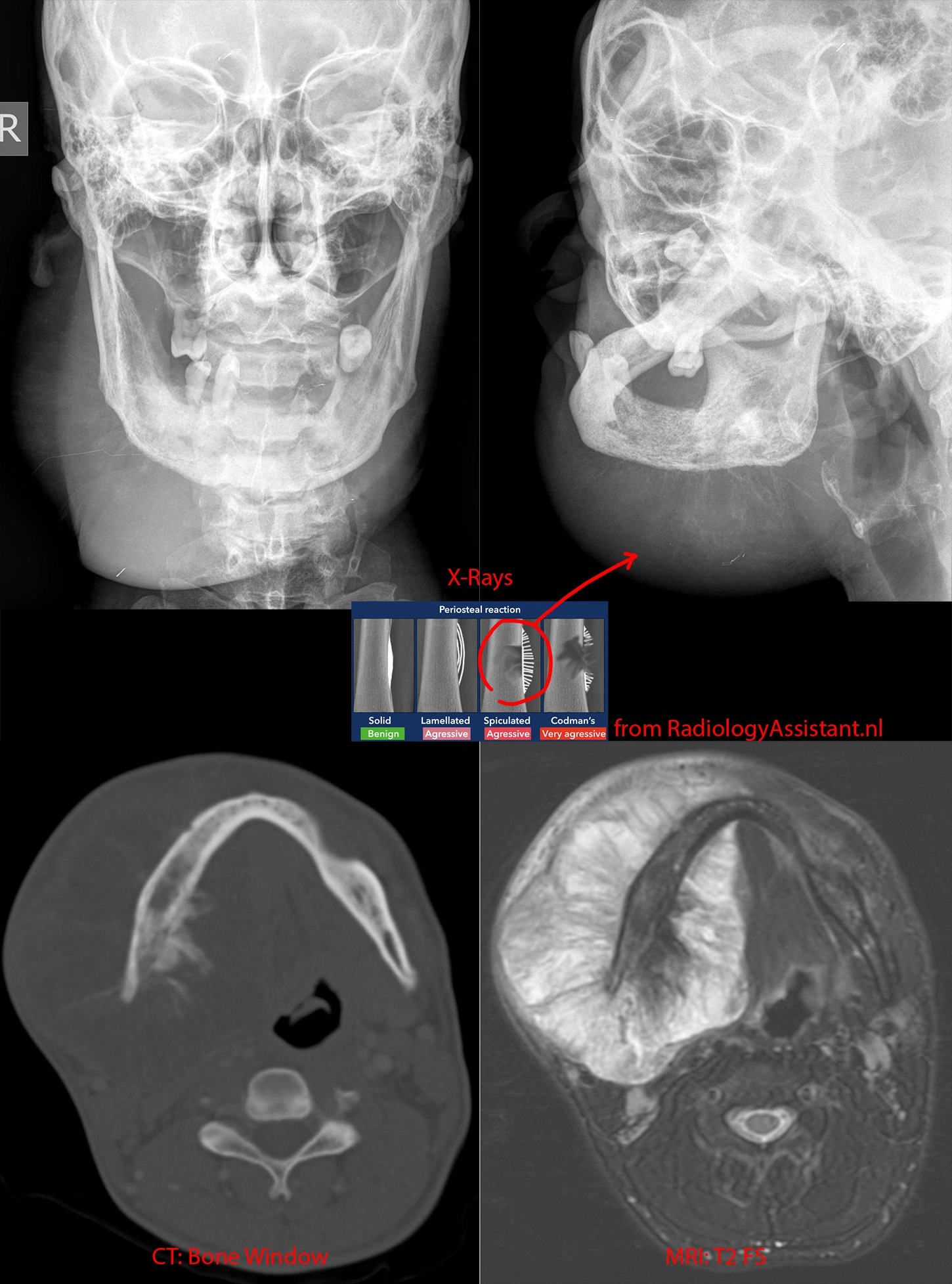
Top left and right: X-rays showing a BIG right jaw mass. Whispy calcifications likely represent spiculated periosteal reaction, a very aggressive bony reaction.
Bottom left: CT in the bone/calcification window shows the periosteal reaction better.
Bottom right: MR in the T2 sequence shows the full extent of the jaw mass and how it extends far beyond the mandible's margins, both outward and inward into the floor of mouth.
While this mass is very large, in general, jaw osteosarcoma has a better prognosis than conventional osteosarcomas.
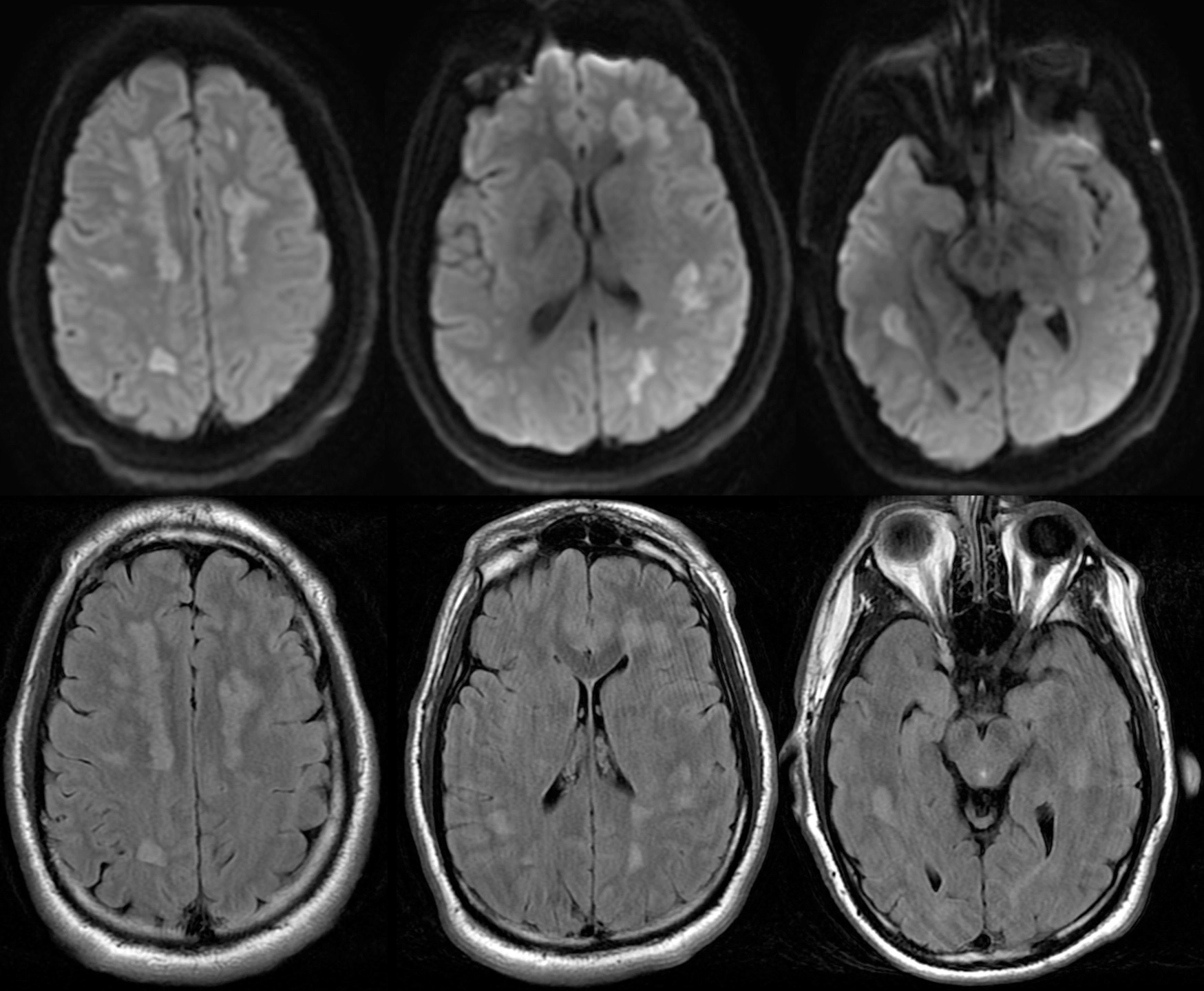
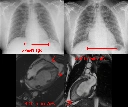
Brain Abscess.

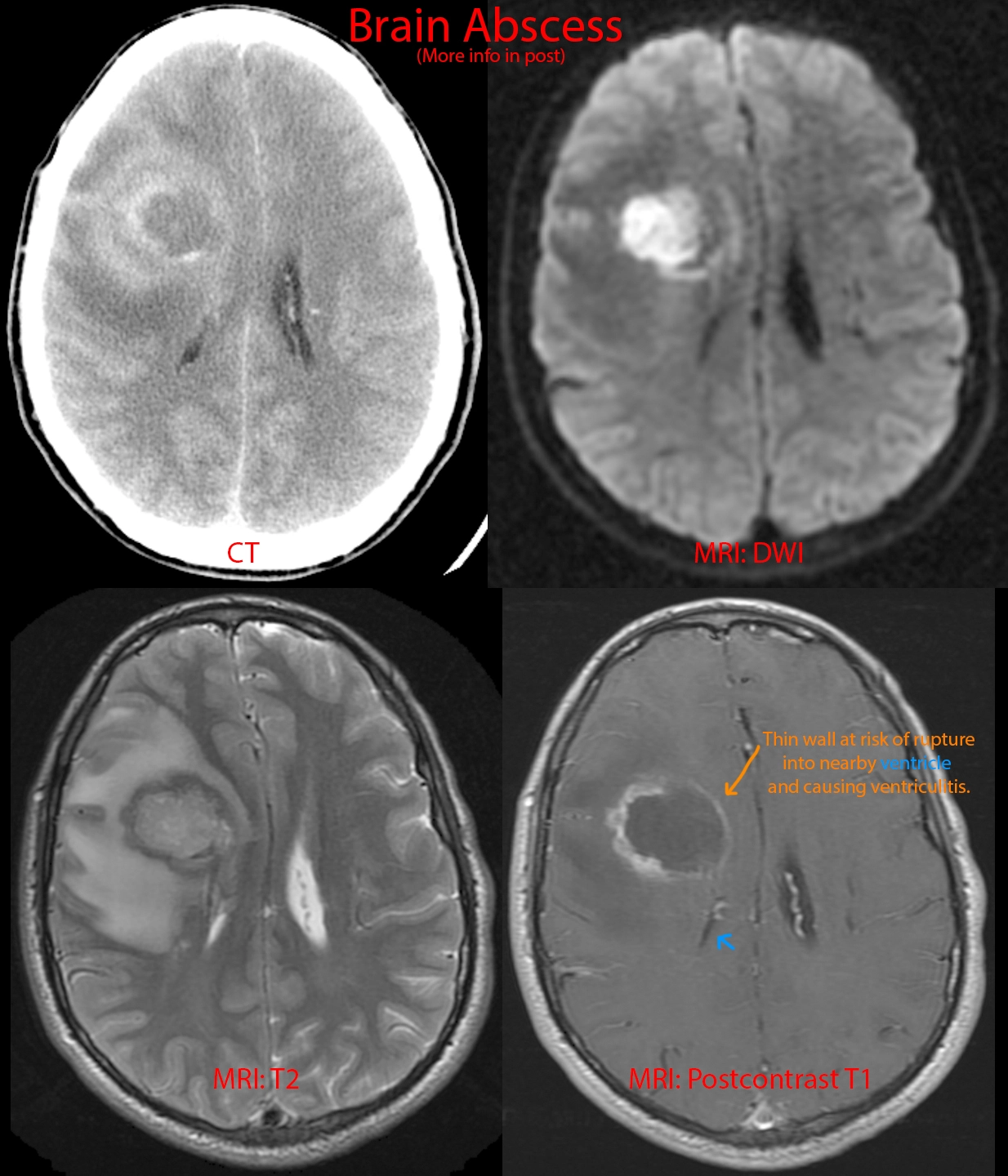
28 year old male with a history of complex congenital heart disease presenting with altered mental status.
CT [top right image]: 4 cm centrally necrotic mass and prominent surrounding brain edema. Ddx: abscess versus tumor.
DWI [top left image]: True diffusion restriction within the central part of the mass, suggesting pus.
T2 [bottom right image]: Great example of the bright-dark-bright arrangement of abscesses on the T2 sequence (bright center, dark abscess capsule, bright surrounding edema).
Postcontrast T1 [bottom left image]: The abscess capsule appears as rim enhancement. The thin medial wall of the abscess [orange arrow] is growing every closer towards the adjacent lateral ventricle [blue arrow] and will ultimately rupture into the ventricle, causing ventriculitis, a high mortality situation.
This patient required surgical drainage of the abscess. The bacteria responsible was a Streptococcus species. Congenital heart disease is a risk factor for cerebral abscesses.