Search
Painful left shoulder.

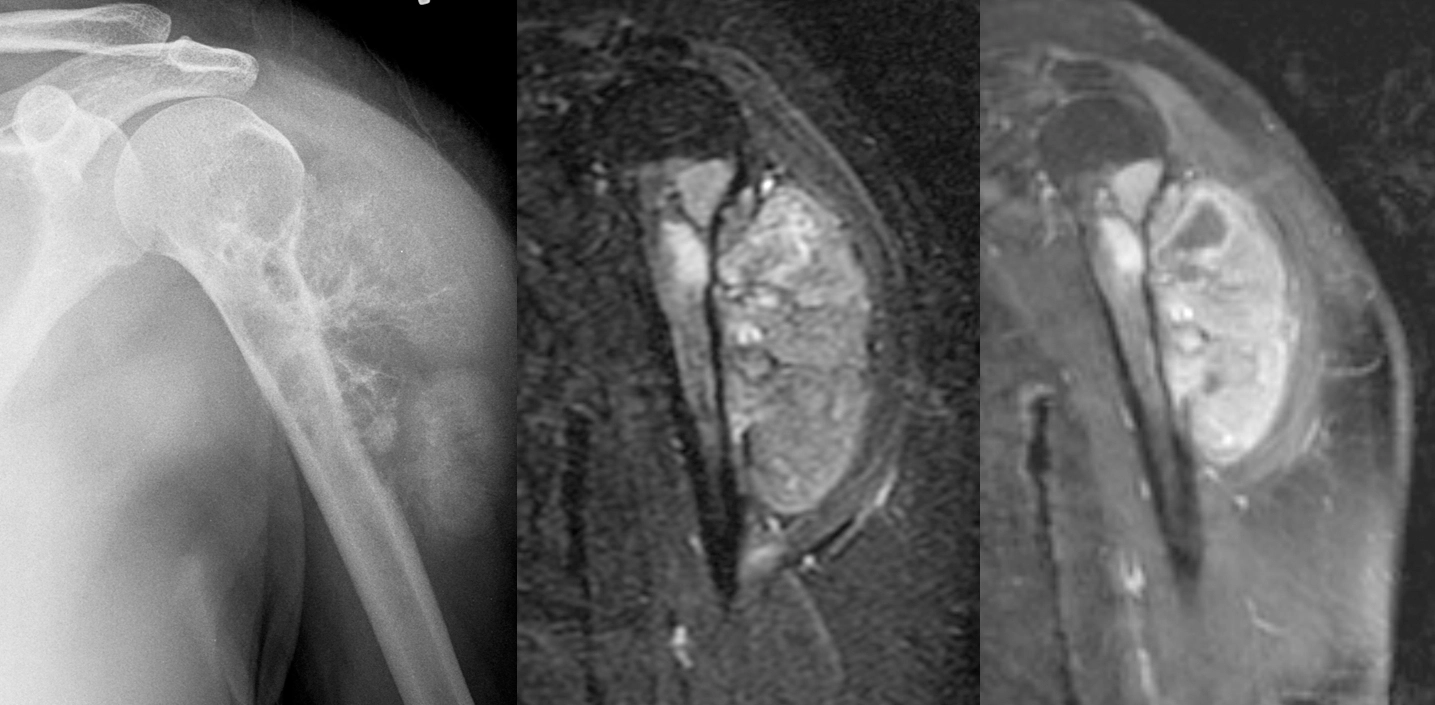
Female in her 30s with painful left shoulder.
[Left]: X-ray shows a mass arising from the left proximal humerus and extending into the adjacent shoulder soft tissues with really aggressive periosteal reaction ("hair on end"). The proximal humerus itself is also heterogeneous with lucent areas. The lateral surface of the upper humerus shows "saucerization," where the cortex is thinned out and looks like a saucer seen on edge.
[Middle]: MRI IR sequence shows a hyperintense bony mass with large soft tissue component.
[Right]: MRI postcontrast T1 IDEAL shows that the mass is enhancing.
This turned out to be high-grade surface osteosarcoma.
10 year old with insidious onset of right medial thigh pain.

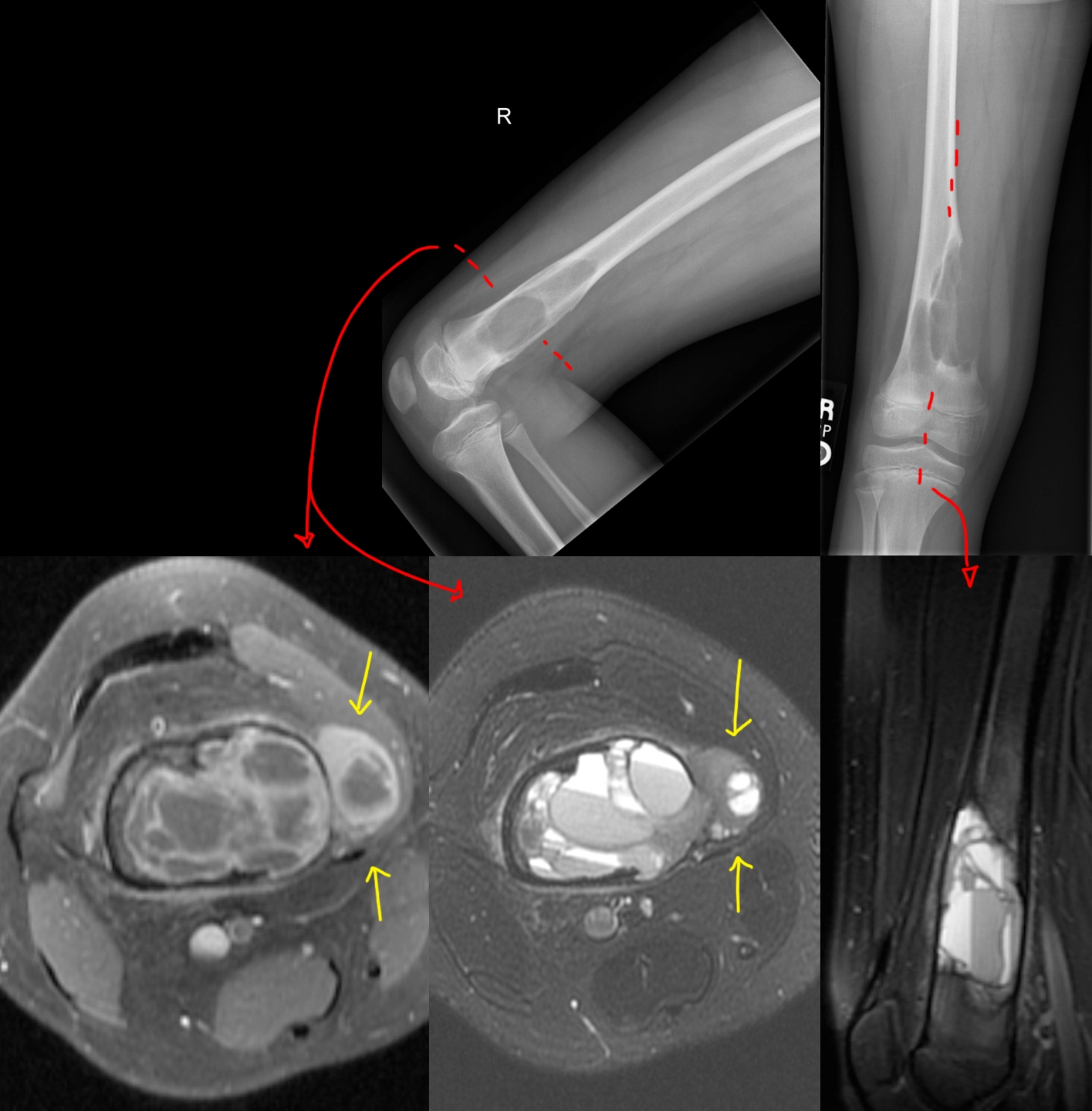
[Top]: X-ray shows a lucent, bubbly, lesion of the distal femur at the metaphysis. On the frontal view [top right], there is breakage through the medial femoral cortex into the adjacent soft tissues, not a good sign.
[Bottom]: MRI shows a multicystic lesion filling the distal femur containing multiple locules, many with fluid-fluid, fluid-debris, and fluid-hemorrhage levels. The most common lesions with this striking appearance are aneurysmal bone cyst, giant cell tumor, or telangiectatic osteosarcoma. Unfortunately, there is clearly extension of the bone tumor beyond the bone (yellow arrows), which favors a more aggressive neoplasm from that differential diagnosis - this turned out to be telangiectatic osteosarcoma.
5 year old who fell off a slide with an unexpected finding.


5 year old who fell off a slide.
Initial imaging shows a comminuted fracture through the distal humerus, compatible with a supracondylar fracture. Nothing else appreciable here, except maybe in retrospect some lucency of the distal humerus where the fracture is.
4- and 7-month follow-up radiographs shows a growing lucent lesion of the distal humerus, expanding the bone there. It has a multicystic appearance. A diagnosis of large simple bone cyst versus aneurysmal bone cyst was proposed.
12 month follow-up was done after the cyst was opened surgically, its contents scraped off, and the resulting cavity was packed with allograft bone chips. At surgery, this turned out to be an aneurysmal bone cyst.
5 year follow-up shows involution of the cyst cavity with some residual heterogeneity and a bone spur at the anterior aspect of the distal humerus.
Abdominal distention despite being told her uterine fibroids "shrunk" after menopause.

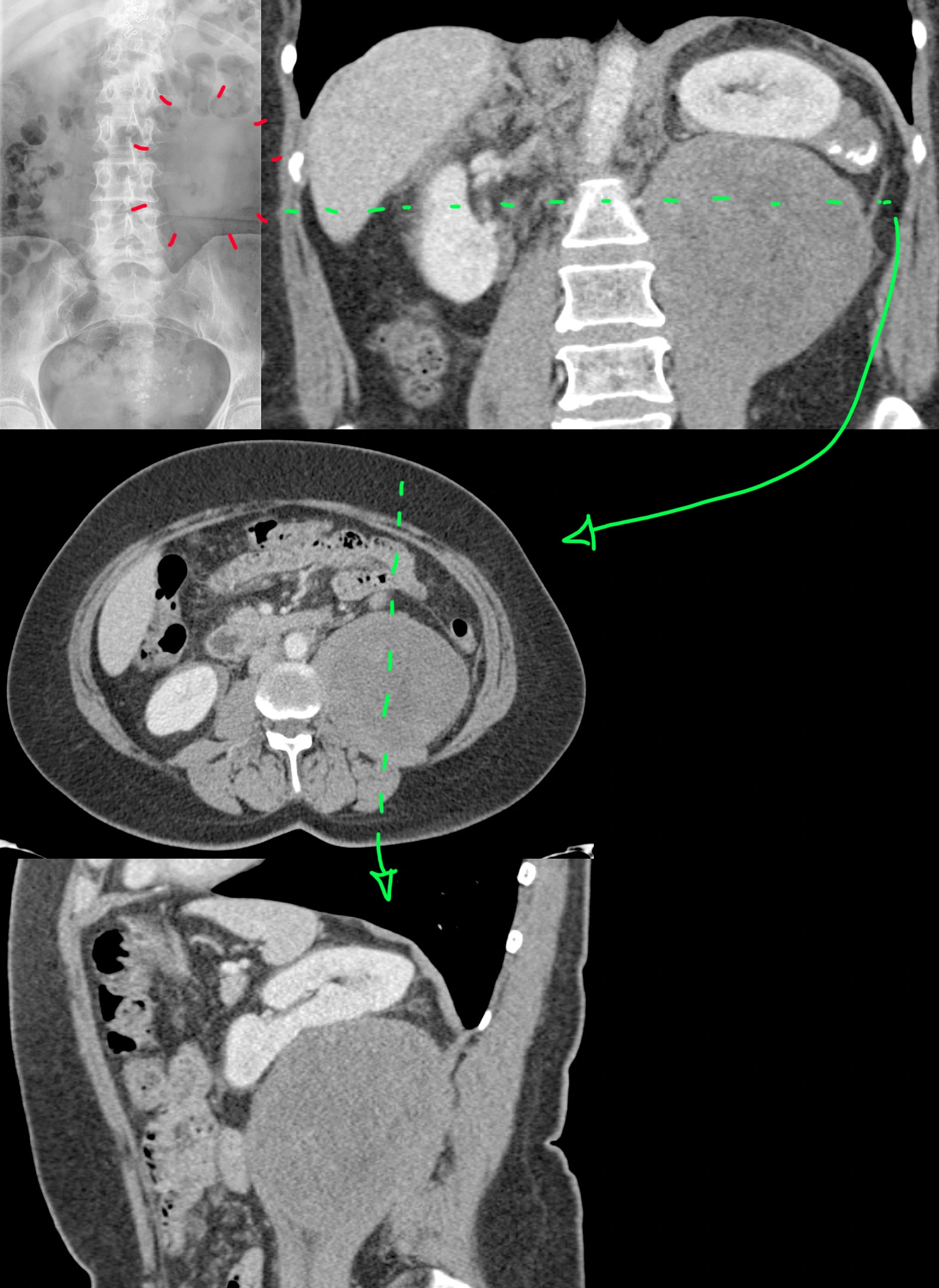
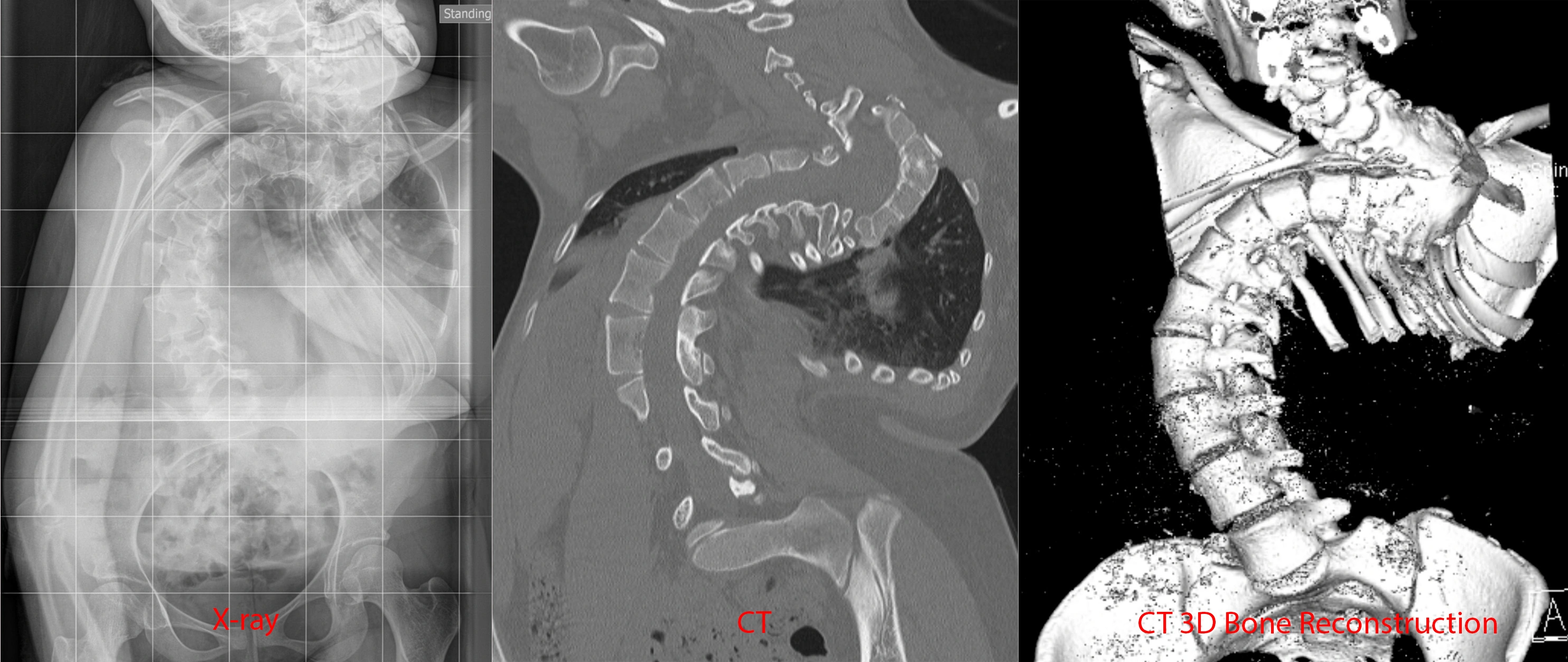
54 year old female with a history of uterine fibroids with persistent abdominal distention despite being told her fibroids shrunk after menopause - presumably via some pelvic ultrasound, which we didn't have.
Abdominal X-ray [top left] was possibly was called normal, which is not completely unreasonable. However, with the help of the follow-up coronal CT [top right], one can see that there is a vague area lacking any bowel gas that looks like it could be a mass. Axial [middle] and sagittal [bottom] CTs show a nonspecific, solid mass, well-circumscribed, with no calcifications, cysts, hemorrhage, or fat inside. The left kidney is pushed up by the mass, but the fat plane between the two is preserved with no evidence of renal invasion.
The patient underwent surgical resection.
Final diagnosis: Retroperitoneal dedifferentiated liposarcoma.
Patient with HIV-AIDS, tapeworm infection, and new fever, cough, fatigue, and weight loss.
This is an absolutely insane case that made the NEJM rounds a couple years ago now. I wish this was mine. I don't think there's been another case report like it since.
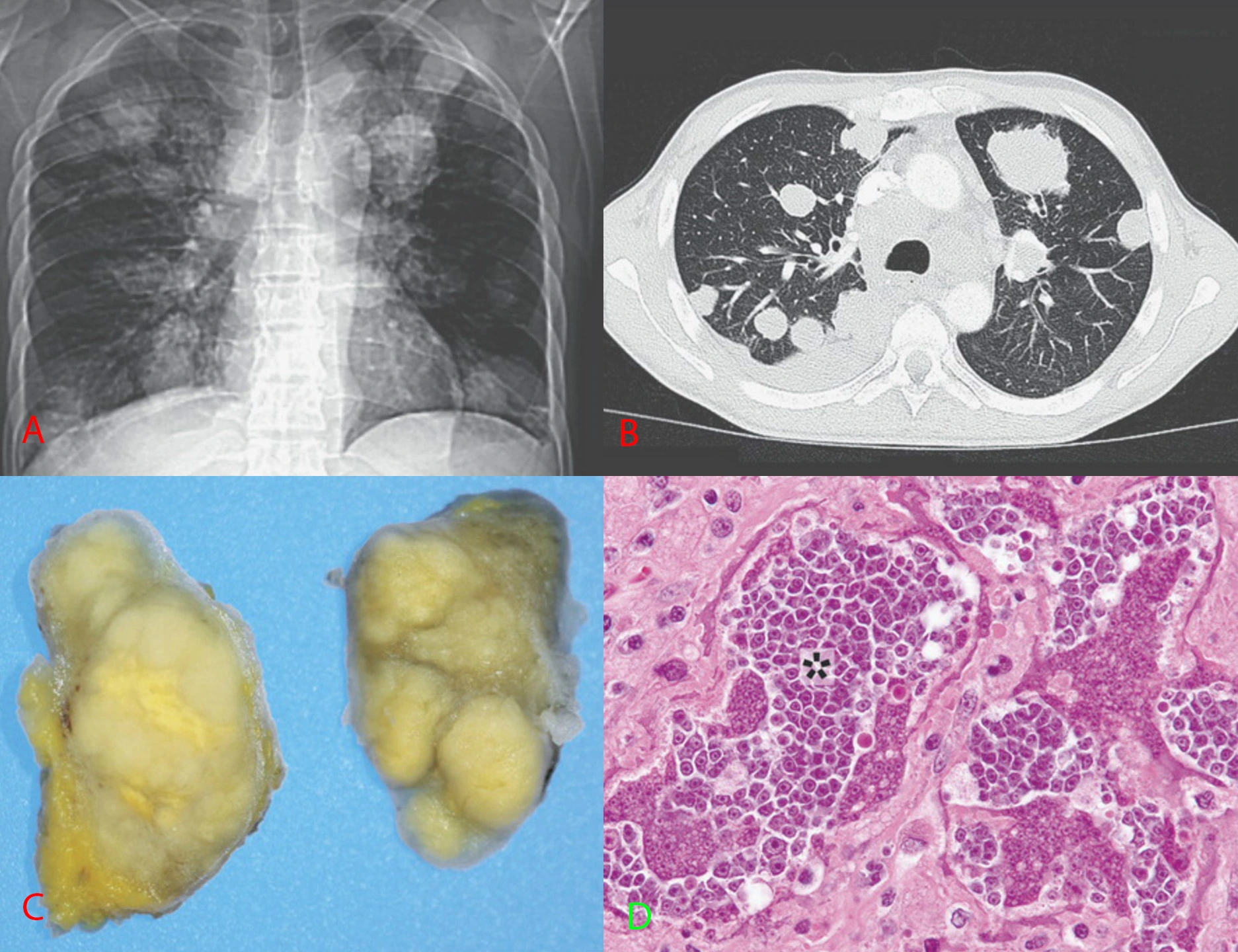
41 year old Colombian male with HIV-AIDS (not adherent to treatment), tapeworm infection, with several months of fever, cough, fatigue, and weight loss.
Top left: Chest x-ray shows multiple round lung masses.
Top right: Chest CT shows those round lung masses. Look like metastases.
Bottom left: The tumors taken out.
Bottom right: Pathology of the tumors.
The patient underwent empiric treatment for tapeworm and HIV with progression of masses. The CDC was contacted for help when treatment wasn't working.
The tumor cells clearly looked like cancer but were too small to be human cells. Genetic sequencing ultimately showed tapeworm DNA, with mutations and genetic rearrangements compatible with cancer.
Final diagnosis: Metastatic tapeworm cancer, likely developed because the patient had no immune system from the HIV-AIDS.
The patient passed away a few days after the diagnosis was finally made.
52 year old who keeps getting pneumothoraces.
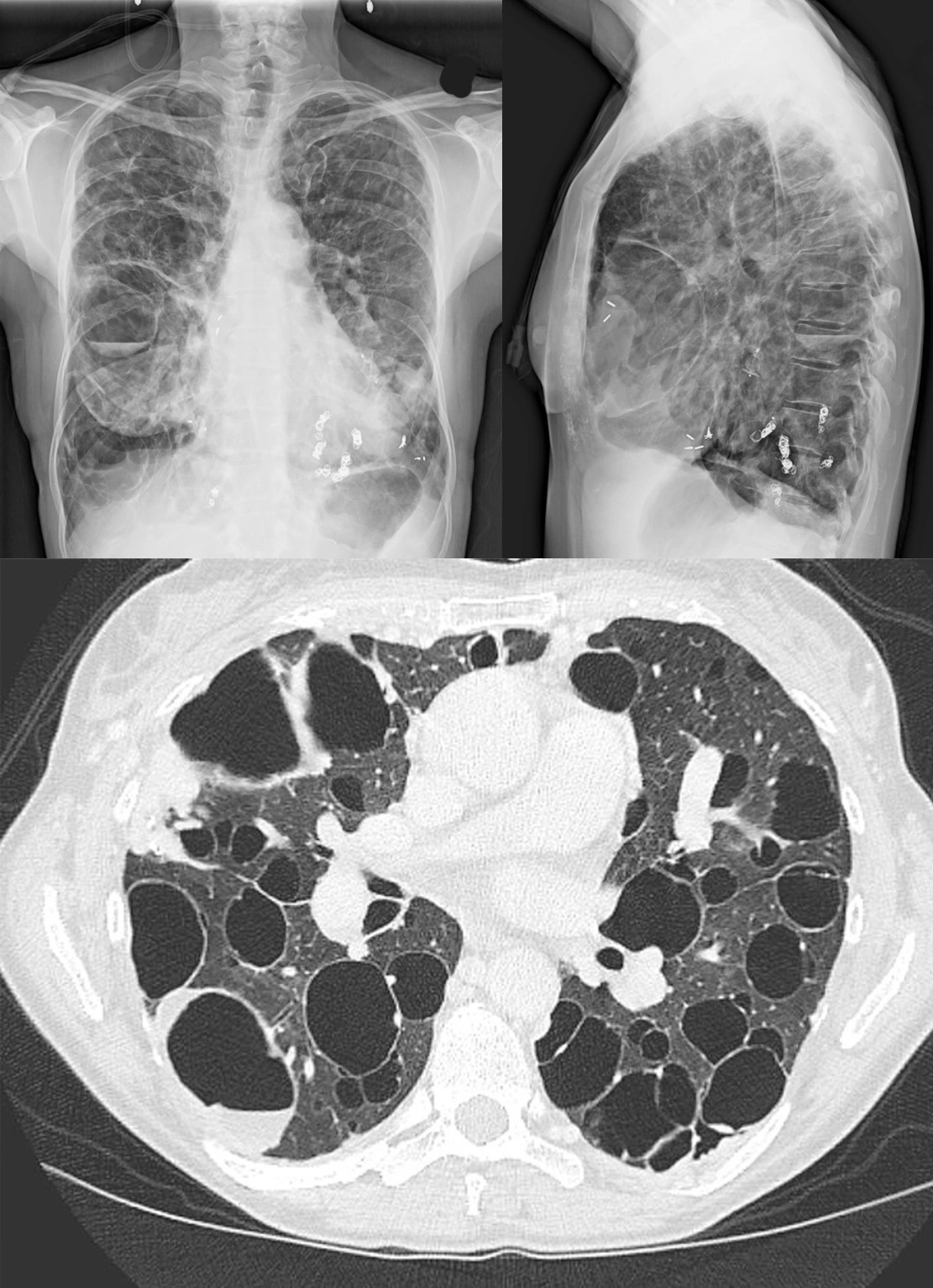
52 year old with a remote history of a rare skin cancer, dermatofibrosarcoma protuberans (DFSP) now presenting with recurrent pneumothoraces and difficulty breathing.
Top: Frontal and lateral chest radiographs shows the lungs filled by numerous cysts of varying sizes. Some cysts have layering fluid in them forming fluid levels.
Bottom: Axial CT through the mid lungs shows the numerous cysts, some with layering fluid, some with wall thickening.
Differential diagnosis for cystic lung disease: airway disease (emphysema, bronchiectasis from various causes), infectious/inflammatory (abscesses, vasculitis), cellular proliferation (cystic metastases, papillomatosis, mesenchymal cystic hamartomas, eosinophilic granulomas, lymphangioleiomyomatosis), injury (traumatic cysts, old lung infarcts).
Final diagnosis: The history of a histiocytic skin cancer suggested an extremely rare entity for cystic lung disease called pulmonary cystic fibrohistiocytic tumor.
It is sort of unclear if the lung cysts represent metastases from the fibrous histiocytic skin cancer or a separate primary neoplasm. The disease has an indolent progressive course. There is no good treatment for this as far as I am aware. These patients also get pulmonary arteriovenous malformations that might need embolization - you can see this patient does have a few embo coils on the chest radiographs at the left lung base.
New shortness of breath on exertion with no past medical history.
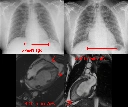
59 year old with no past medical history, now with new dyspnea on exertion.
Top: Chest radiographs show development of cardiomegaly since 6 years prior. The pulmonary vascular markings are also more prominent than before, suggesting pulmonary congestion.
Bottom: MRI Cine FIESTA sequences in the 4- and 2-chamber views at end-diastole. There are prominent trabeculations towards the cardiac apex at both the left and right ventricles. In particular, there is an outer layer of dense myocardium and a thicker inner layer of trabeculated myocardium.
Final Diagnosis: Cardiac noncompaction.
Comparison Case: Meth-Induced Cardiomyopathy.
Cardiac noncompaction is a genetic disorder leading to failure of the myocardium to form "compact" walls. It is extremely rare. The presentation depends on how bad the noncompaction is, so can be asymptomatic to heart failure, arrhythmias, and thromboembolism.
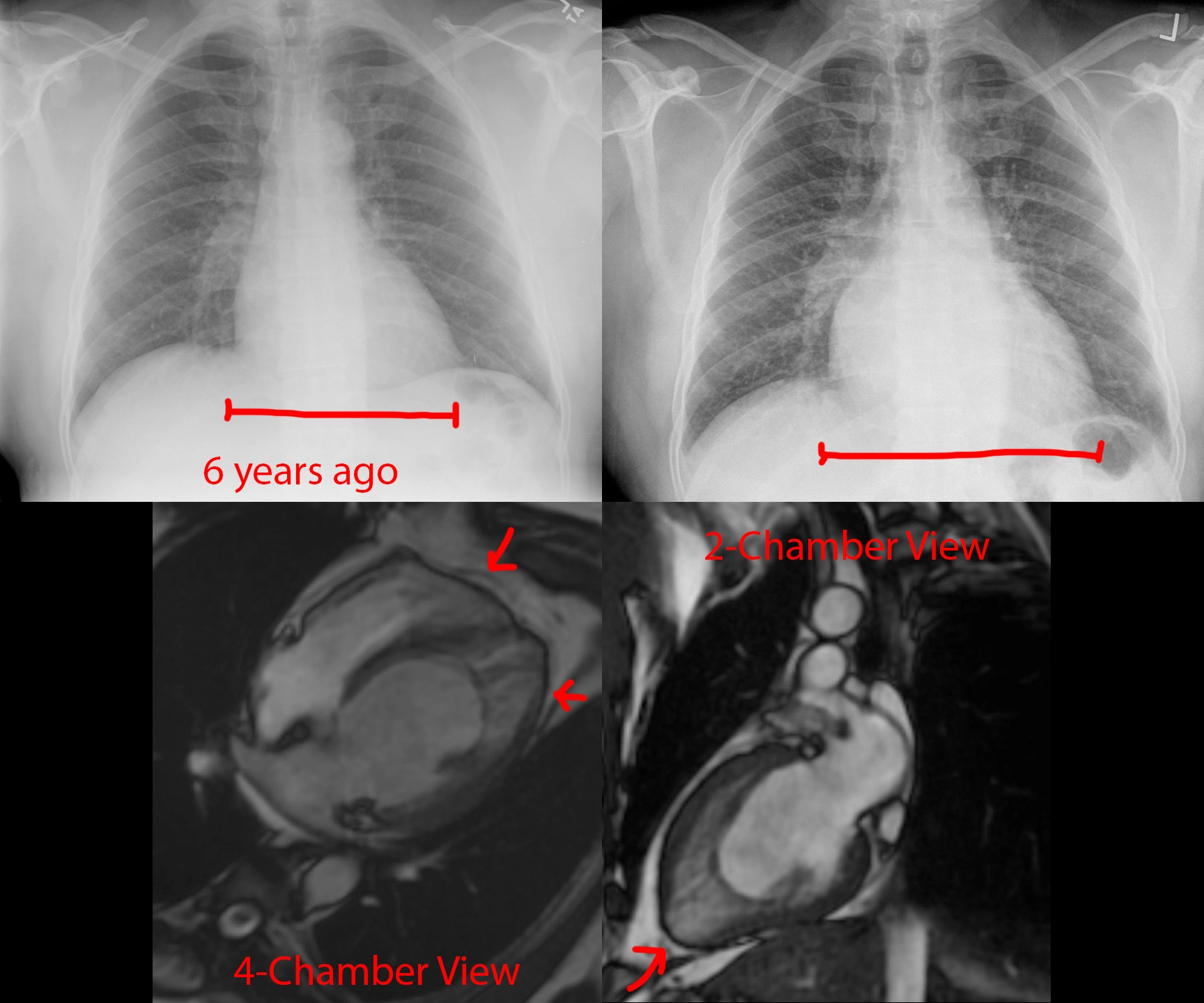
Gnathic (jaw) osteosarcoma.

Top left and right: X-rays showing a BIG right jaw mass. Whispy calcifications likely represent spiculated periosteal reaction, a very aggressive bony reaction.
Bottom left: CT in the bone/calcification window shows the periosteal reaction better.
Bottom right: MR in the T2 sequence shows the full extent of the jaw mass and how it extends far beyond the mandible's margins, both outward and inward into the floor of mouth.
While this mass is very large, in general, jaw osteosarcoma has a better prognosis than conventional osteosarcomas.
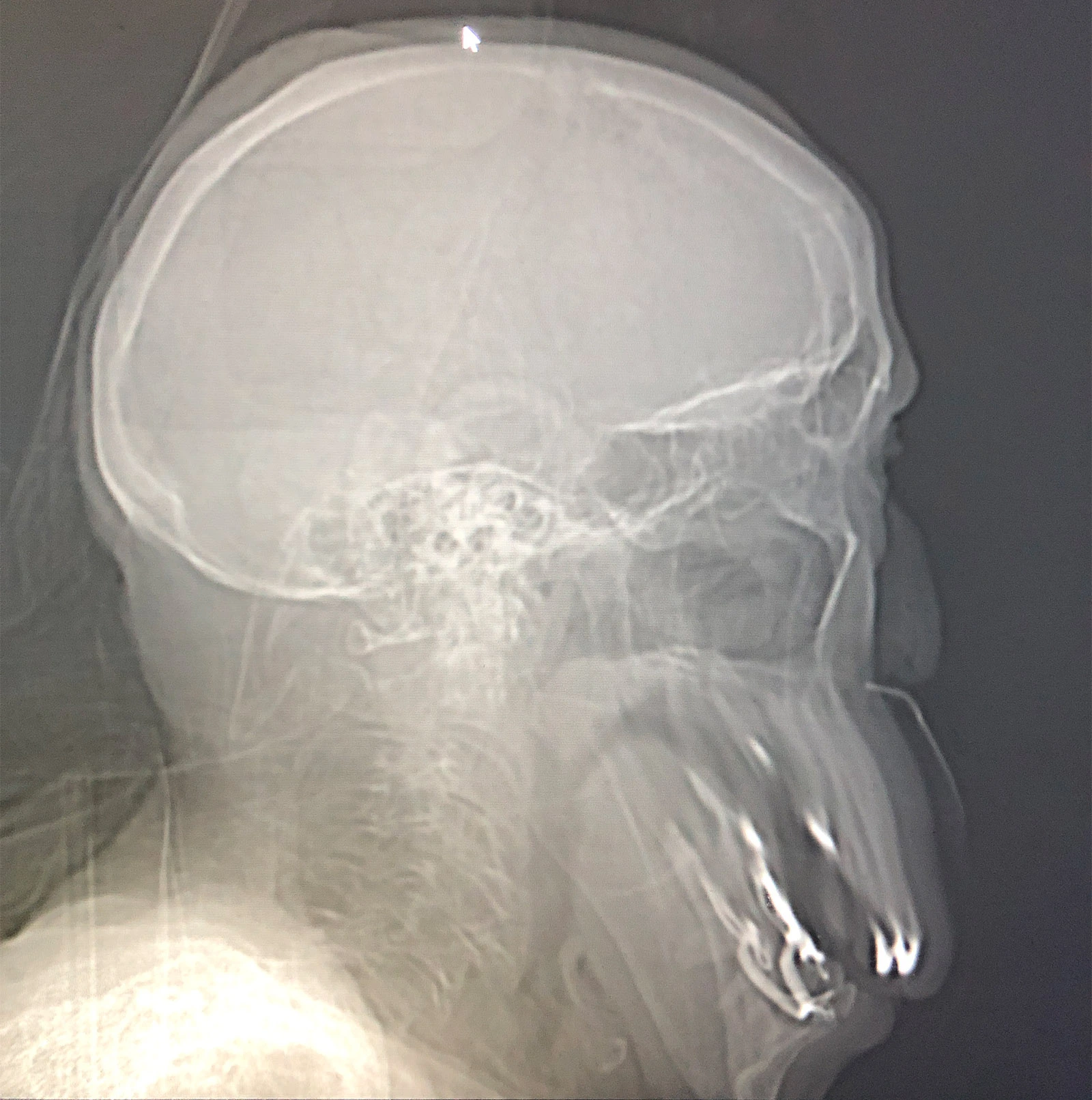
Innumerable skull lesions of multiple myeloma.
Two different patients, both aged 59, with known multiple myeloma.
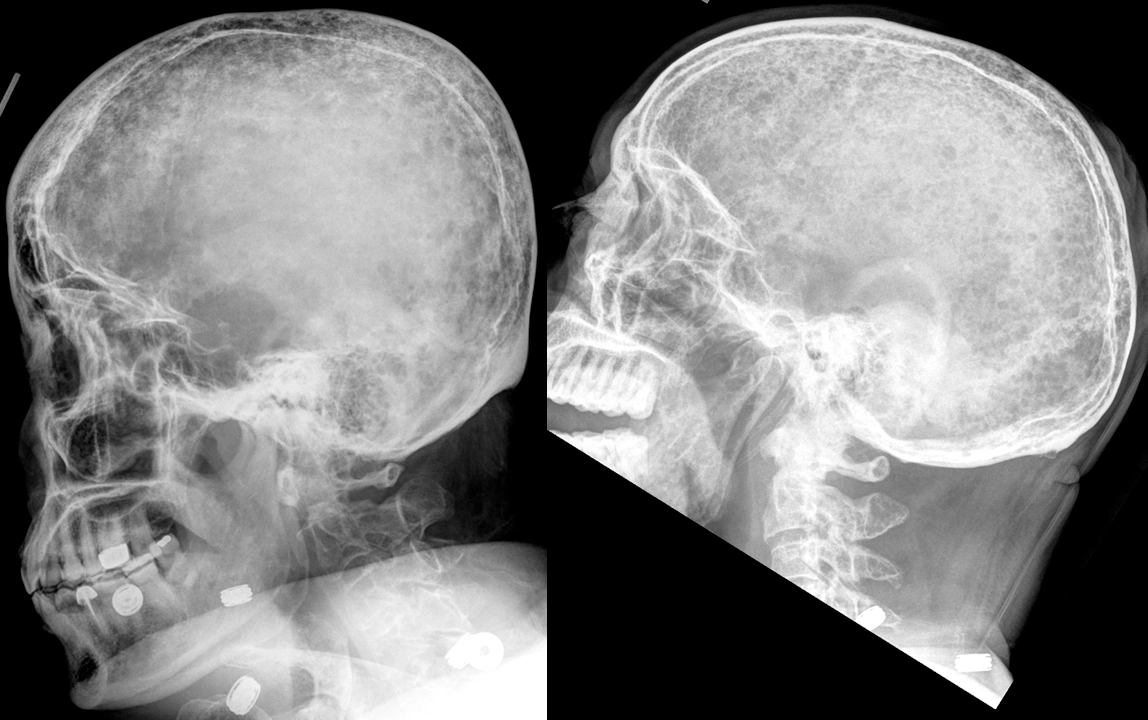
Codman's triangles in osteosarcoma.

7 year old with conventional (intramedullary high-grade) osteosarcoma of the femur.
X-ray shows an aggressive bone lesion with Codman's triangles and extension into the adjacent soft tissues.
MRI shows the full extent of the tumor much better - it is involving the full thickness of the femur, has much further soft tissue extension than suggested by the Codman's triangles, and even extends into the soft tissues on the other side.
Cystic lung disease of trisomy 21 (Down syndrome).
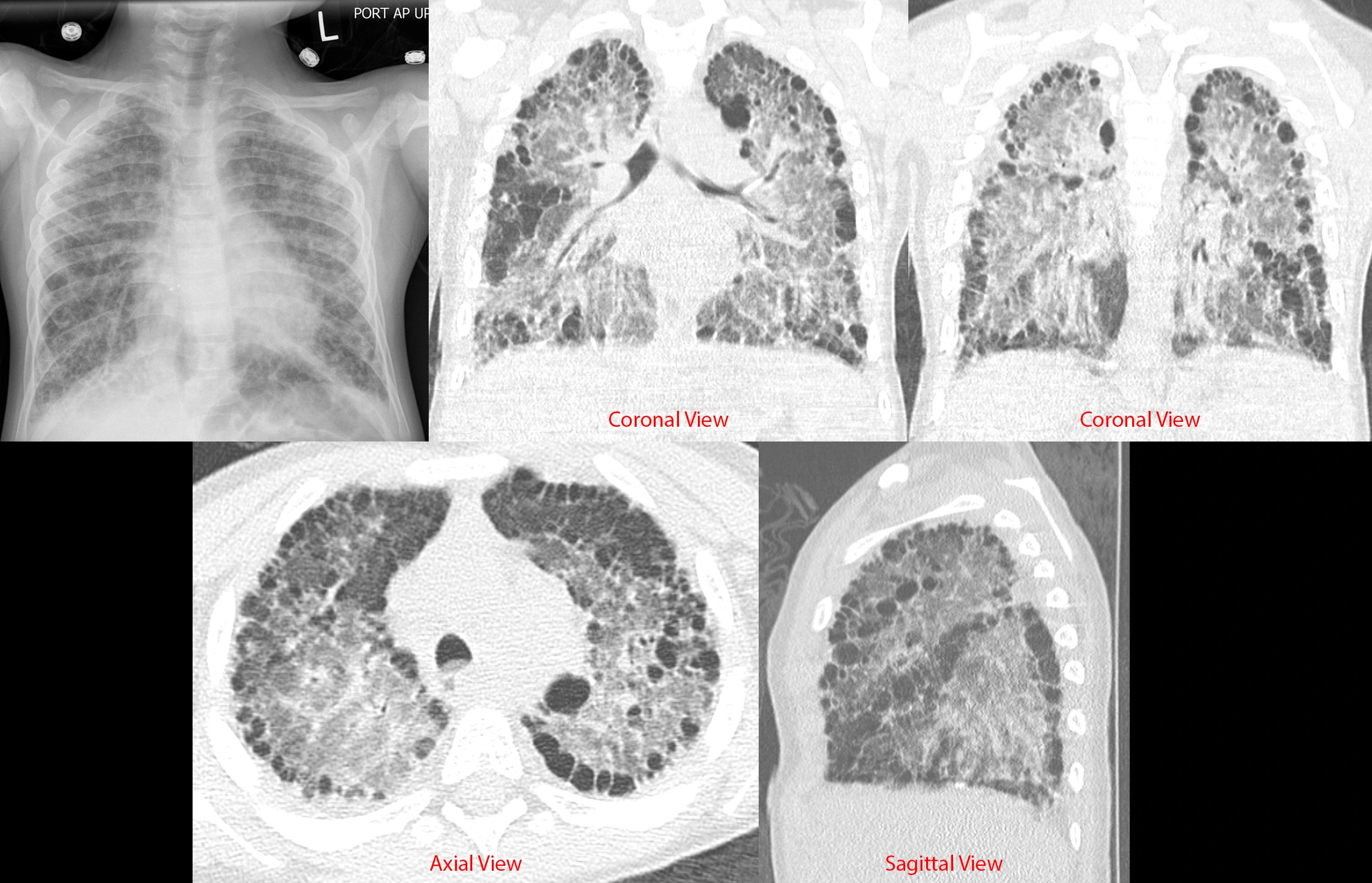
8 year old with a history of trisomy 21 (Down syndrome) with tachycardia.
Chest x-ray shows prominent interstitial markings and cystic changes throughout the lungs. An atrial septal defect occlusion device is present.
CTs show prominent interstitial markings and ground glass opacities as well as numerous cysts that are predominantly subpleural (peripheral) in location.
Cystic subpleural changes are a known finding of trisomy 21, although with a relatively limited number of reports in the literature. This patient likely also has additional chronic lung disease based on the presence of the interstitial markings and ground glass opacities that may be related to prematurity or prior infectious/inflammatory processes.
Diagnosis - Lululemon.

If you're planning on getting an MRI, avoid wearing Lululemon, especially their silver-impregnated stuff - the strong changing magnetic fields can cause the clothing to heat up to the point of causing burns (just Google for news articles).
Pectus excavatum and its treatment.

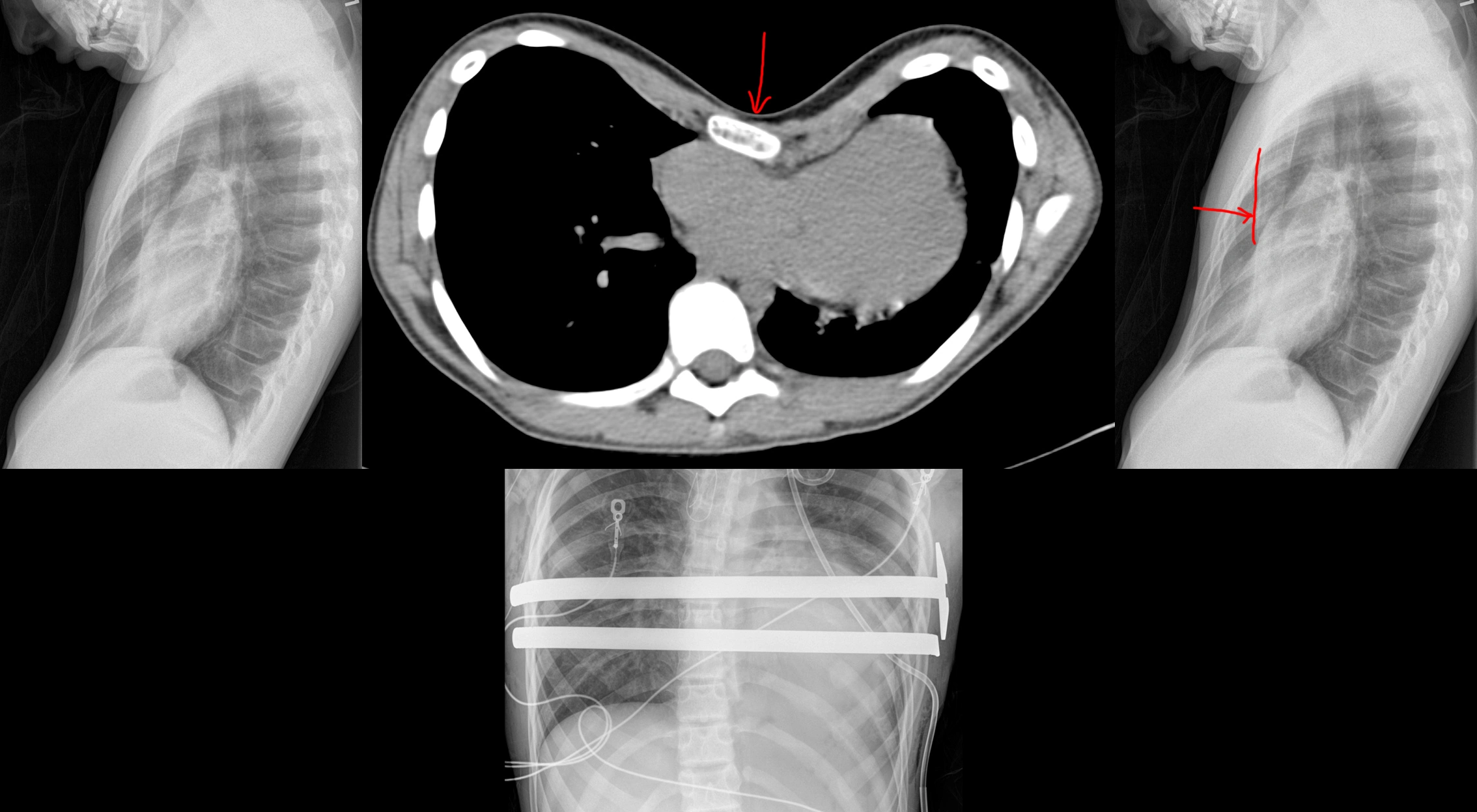
12 year old with pectus deformity causing fatigue and chest pain. CT shows the really deep sternum indenting the heart. Cardiac echo (not shown) reported right ventricular compression to the point it was affecting systolic function. The patient had Nuss bars placed to correct the deformity.
The classic internet rectal foreign body... or is it?

On the left side, 2 x-rays of 2 different patients with 2 different objects in their pelvis. Internet denizens would no doubt instantly diagnose these as accidental rectal foreign bodies from people falling on their butts. However, these are both pessaries used to treat pelvic organ prolapse. The top one is an inflatoball pessary. The bottom one is a ring-shaped pessary that we see on edge.
Life's middle finger: malignant melanoma.

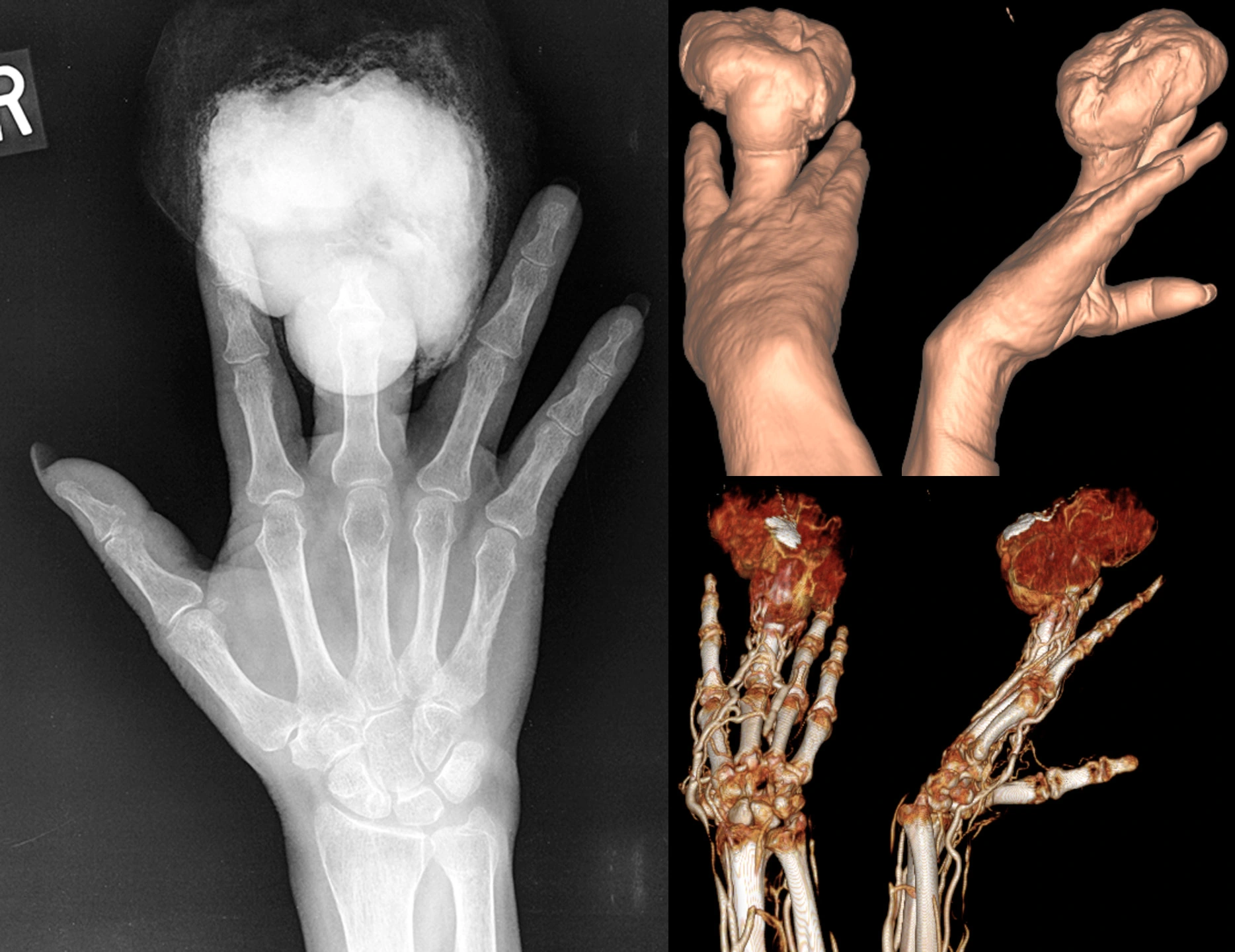
54 year old female with a history of minor injury to the finger 6 months before these studies were obtained, subsequently developed an infection requiring debridement. The wound was then stable until 2 months before, when a large, fungating, hemorrhagic mass grew.
X-ray shows large radiopaque mass eroding the distal finger (distal phalanx and distal portion of the middle phalanx).
CT 3D surface reconstructions show the morphology of the mass.
CTA 3D reconstruction shows the mass is very hypervascular.
Lymph node scintigraphy was performed showing a sentinel node at the axilla (not shown). The patient underwent amputation of the finger with axillary sentinel node biopsy, which was positive for metastatic melanoma. The patient was then lost to follow-up.
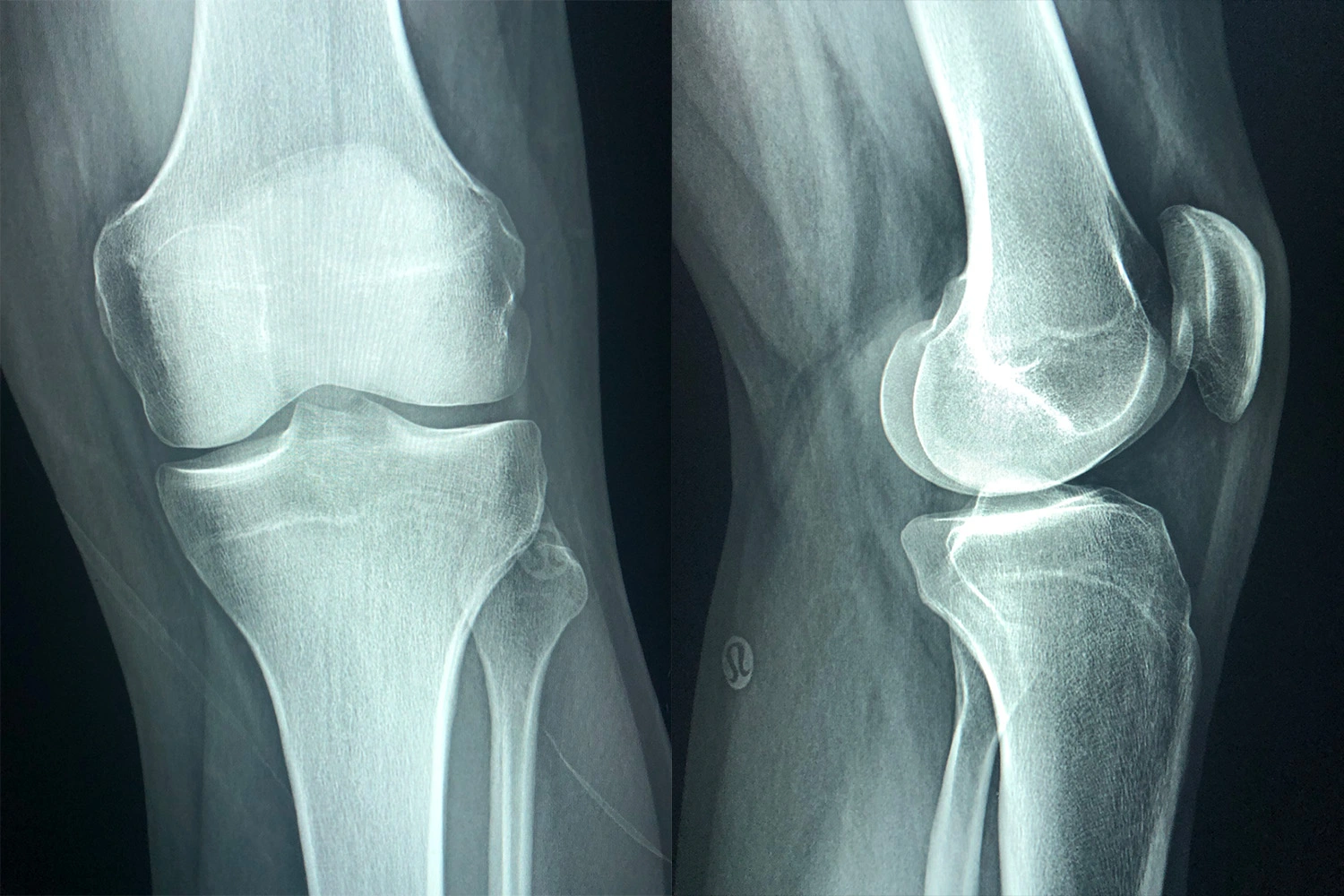
Accidentally fired gun into knee.

38 year old guy fired his 45 mm into his knee while cleaning the gun. No exit wound.
There is a comminuted fracture of the distal femur with multiple bullet fragments, including the largest at the intercondylar notch. There is gas/air in the knee joint, forming air-fluid levels on lateral view. There are additional foci of gas in the surrounding soft tissues.
Patient underwent arthrotomy for foreign body removal and fixation of the supracondylar/intercondylar femoral fracture.
Lethal left ventricular rupture.

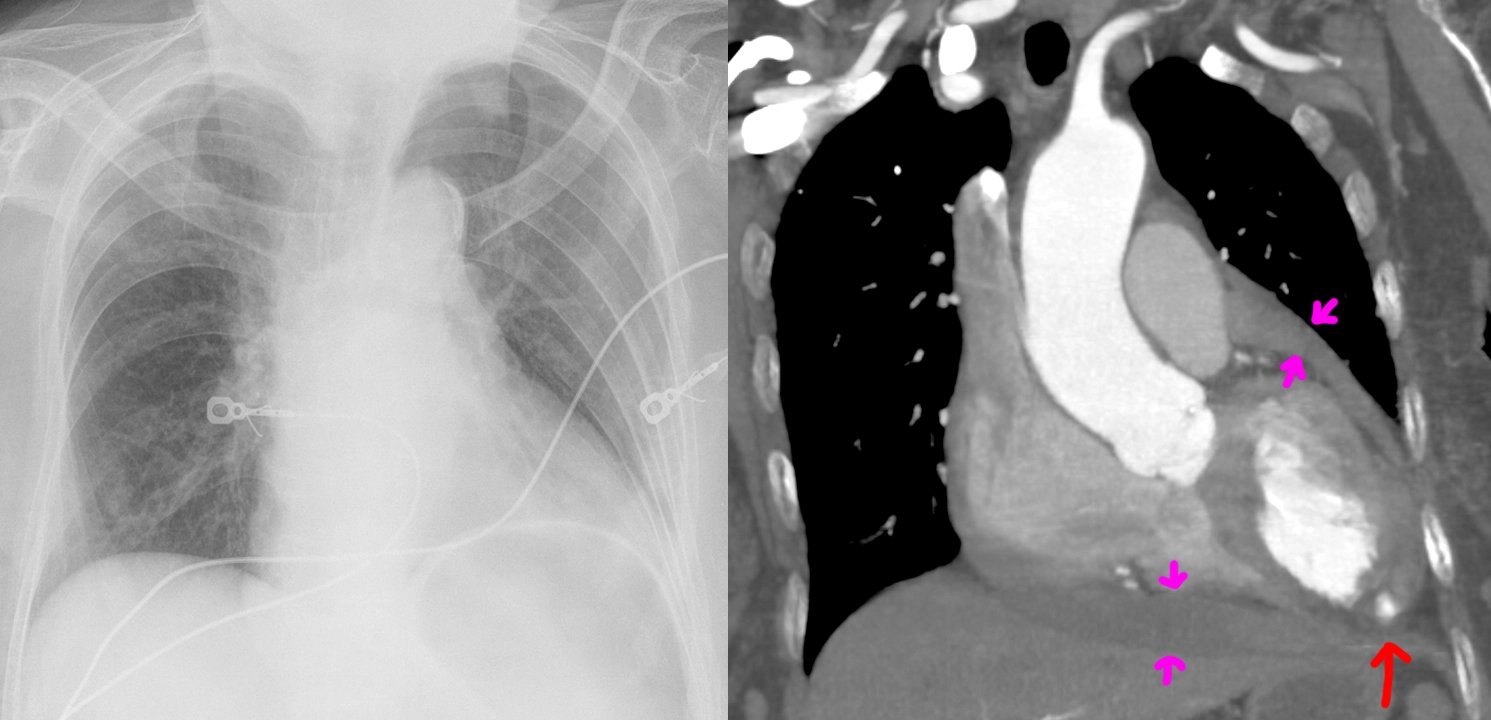
Elderly female with a history of hypertension, stroke, and, 1 month before, heart attack with cardiac arrest. The patient presented to the emergency department with 1 day of nausea, vomiting, cold sweats, and malaise. Troponins 1.54. ECG with inferior Q waves but no ST elevation/depression or T-wave inversion.
Chest radiograph shows an enlarged cardiac silhouette, for which a differential of cardiomegaly or pericardial effusion was suggested, as well as increased pulmonary vascular markings compatible with pulmonary congestion. Compared chest radiograph findings to the images from the methamphetamine-induced cardiomyopathy case.
CT angiography shows both cardiomegaly as well as an intermediate-density pericardial effusion (magenta arrows) concerning for hemopericardium. Most concerningly (holy-shit concerningly), there is a left ventricular aneurysm with rupture and blush of contrast (red arrow) into the hemopericardium, compatible with ongoing bleeding.
It is not surprising that a rupture of the heart carries high mortality risk. The patient passed away from PEA cardiac arrest shortly after admission, likely from cardiac tamponade by the enlarging hemopericardium.
Methamphetamine-induced cardiomyopathy.

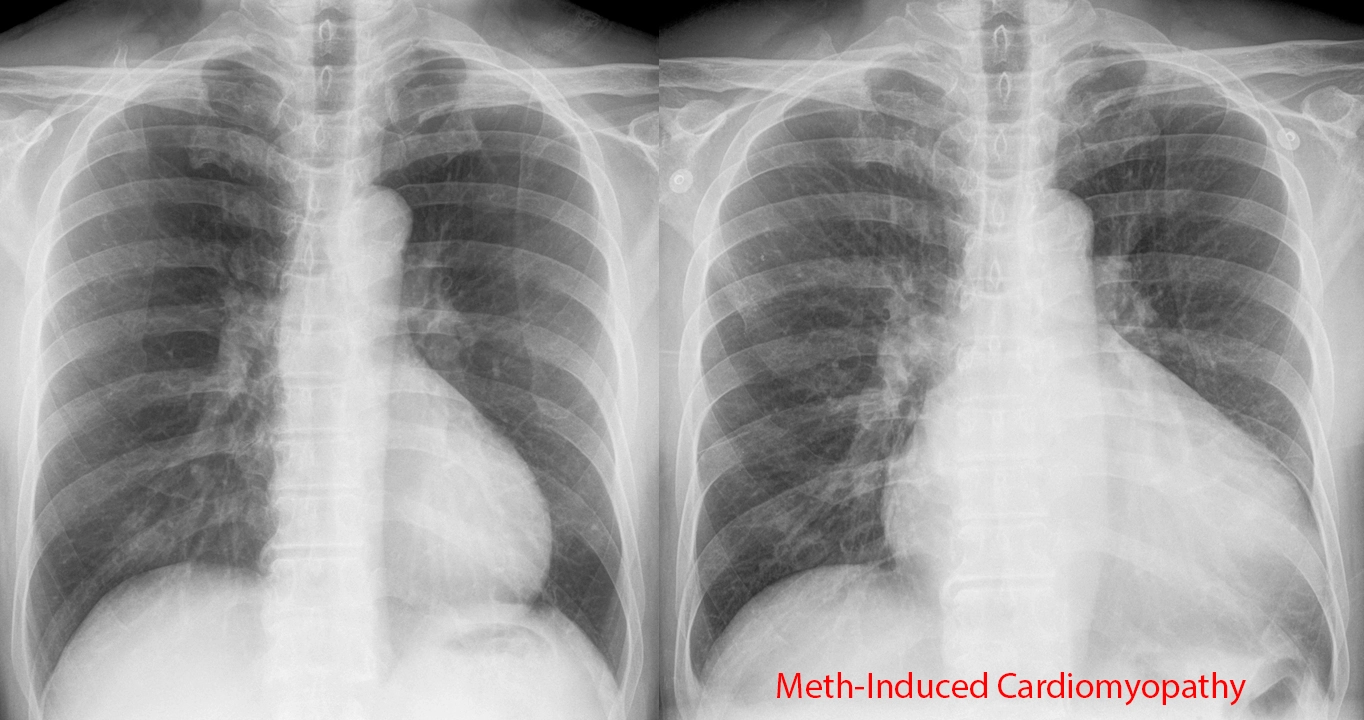
60 year old male with a history of homelessness, latent tuberculosis, and methamphetamine abuse. The patient was admitted to the hospital for shortness of breath and leg edema. A urine drug test on admission was positive for methamphetamine.
Chest radiograph (right) shows an enlarged cardiac silhouette, for which a differential of cardiomegaly or pericardial effusion was provided. Subsequent echocardiogram confirmed this was cardiomegaly with a low ejection fraction. The pulmonary vascular markings on the chest x-ray are also prominent, compatible with congestion from heart failure. The patient has a normal past chest radiograph (left) that provides an easy comparison for these findings.