Search
Patient with HIV-AIDS, tapeworm infection, and new fever, cough, fatigue, and weight loss.
This is an absolutely insane case that made the NEJM rounds a couple years ago now. I wish this was mine. I don't think there's been another case report like it since.
41 year old Colombian male with HIV-AIDS (not adherent to treatment), tapeworm infection, with several months of fever, cough, fatigue, and weight loss.
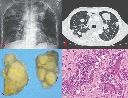
Top left: Chest x-ray shows multiple round lung masses.
Top right: Chest CT shows those round lung masses. Look like metastases.
Bottom left: The tumors taken out.
Bottom right: Pathology of the tumors.
The patient underwent empiric treatment for tapeworm and HIV with progression of masses. The CDC was contacted for help when treatment wasn't working.
The tumor cells clearly looked like cancer but were too small to be human cells. Genetic sequencing ultimately showed tapeworm DNA, with mutations and genetic rearrangements compatible with cancer.
Final diagnosis: Metastatic tapeworm cancer, likely developed because the patient had no immune system from the HIV-AIDS.
The patient passed away a few days after the diagnosis was finally made.
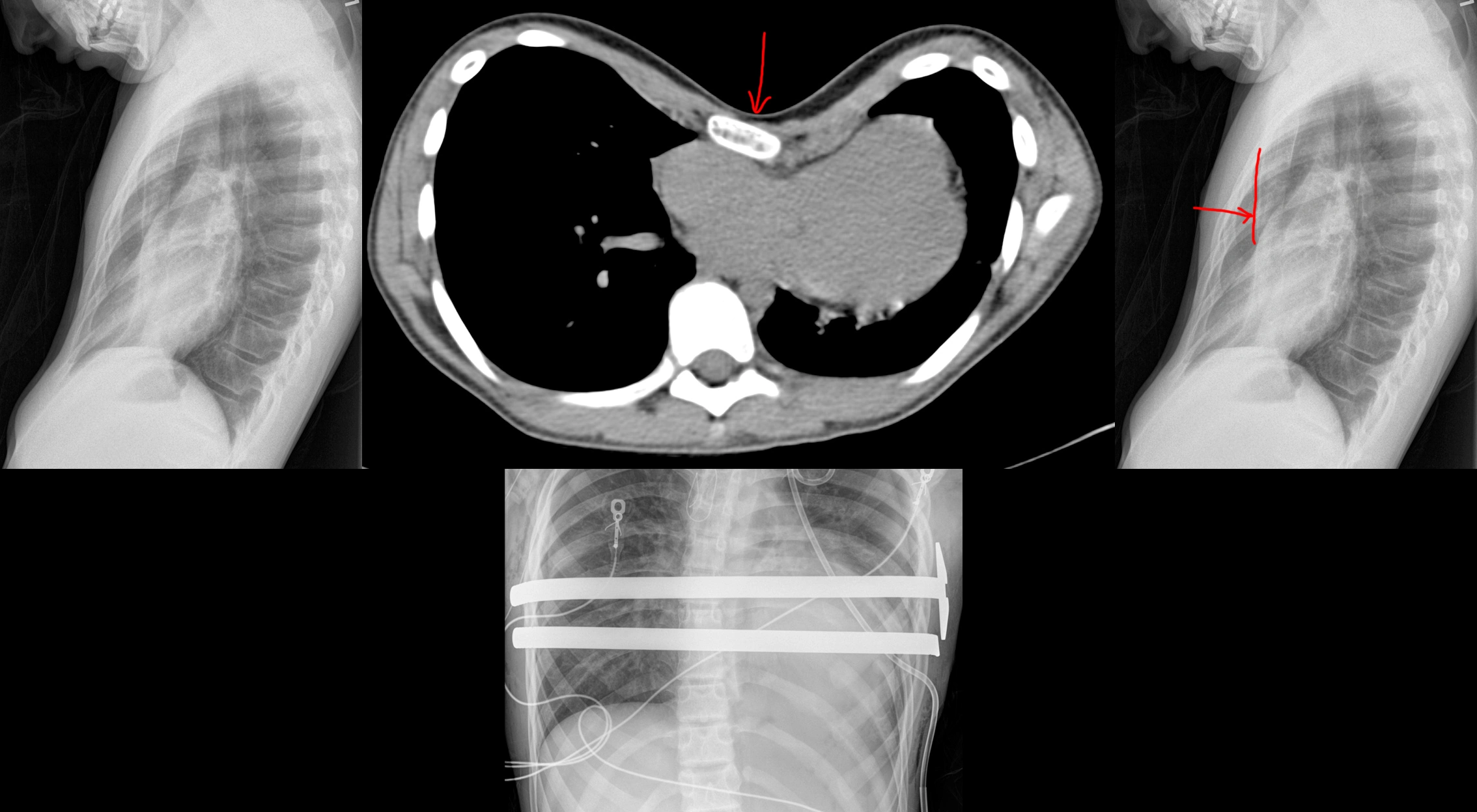
52 year old who keeps getting pneumothoraces.
52 year old with a remote history of a rare skin cancer, dermatofibrosarcoma protuberans (DFSP) now presenting with recurrent pneumothoraces and difficulty breathing.
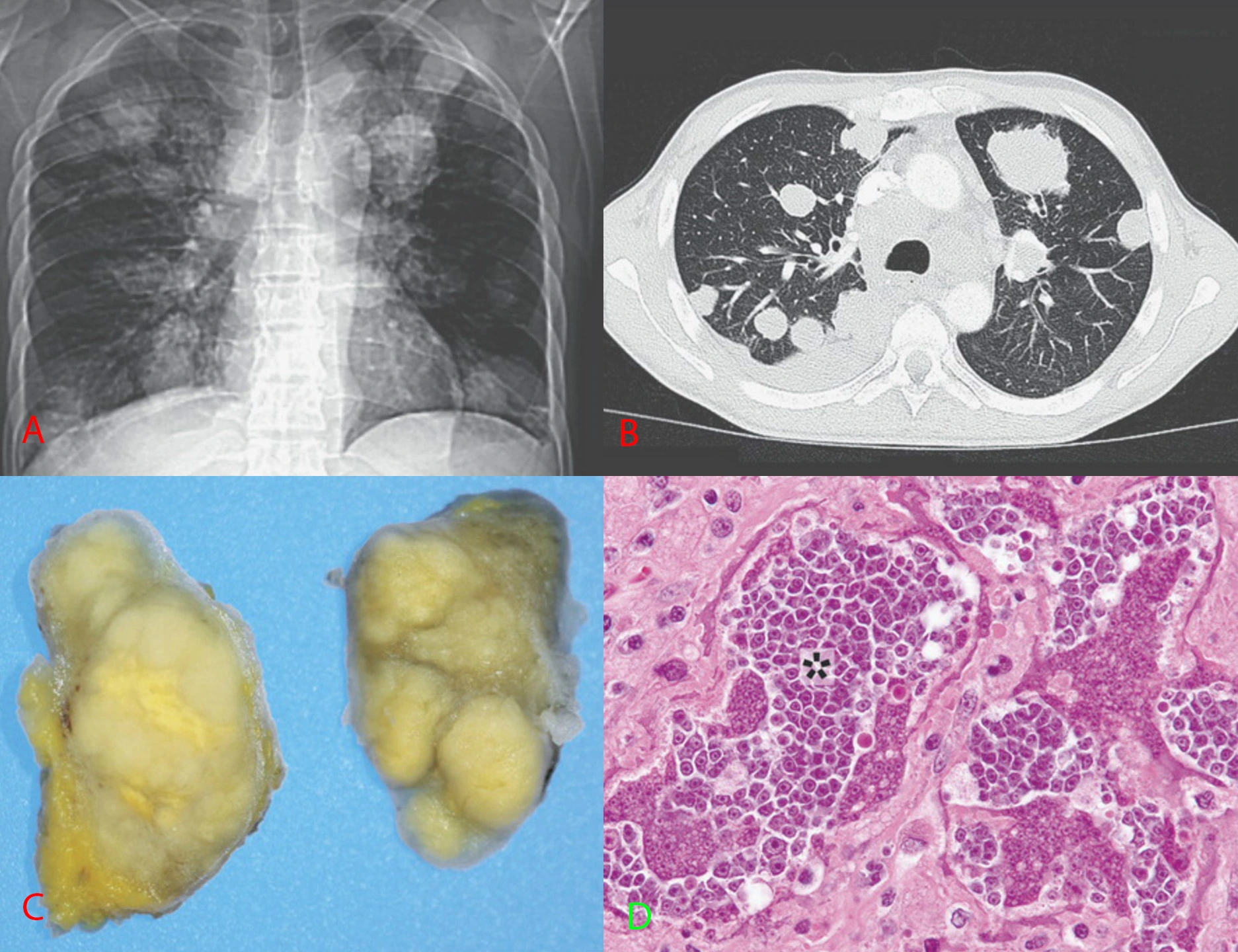
Top: Frontal and lateral chest radiographs shows the lungs filled by numerous cysts of varying sizes. Some cysts have layering fluid in them forming fluid levels.
Bottom: Axial CT through the mid lungs shows the numerous cysts, some with layering fluid, some with wall thickening.
Differential diagnosis for cystic lung disease: airway disease (emphysema, bronchiectasis from various causes), infectious/inflammatory (abscesses, vasculitis), cellular proliferation (cystic metastases, papillomatosis, mesenchymal cystic hamartomas, eosinophilic granulomas, lymphangioleiomyomatosis), injury (traumatic cysts, old lung infarcts).
Final diagnosis: The history of a histiocytic skin cancer suggested an extremely rare entity for cystic lung disease called pulmonary cystic fibrohistiocytic tumor.
It is sort of unclear if the lung cysts represent metastases from the fibrous histiocytic skin cancer or a separate primary neoplasm. The disease has an indolent progressive course. There is no good treatment for this as far as I am aware. These patients also get pulmonary arteriovenous malformations that might need embolization - you can see this patient does have a few embo coils on the chest radiographs at the left lung base.
New shortness of breath on exertion with no past medical history.
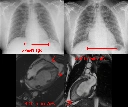
59 year old with no past medical history, now with new dyspnea on exertion.
Top: Chest radiographs show development of cardiomegaly since 6 years prior. The pulmonary vascular markings are also more prominent than before, suggesting pulmonary congestion.
Bottom: MRI Cine FIESTA sequences in the 4- and 2-chamber views at end-diastole. There are prominent trabeculations towards the cardiac apex at both the left and right ventricles. In particular, there is an outer layer of dense myocardium and a thicker inner layer of trabeculated myocardium.
Final Diagnosis: Cardiac noncompaction.
Comparison Case: Meth-Induced Cardiomyopathy.
Cardiac noncompaction is a genetic disorder leading to failure of the myocardium to form "compact" walls. It is extremely rare. The presentation depends on how bad the noncompaction is, so can be asymptomatic to heart failure, arrhythmias, and thromboembolism.
"Crazy coworker stabbed her at her house." (Liver laceration with active bleeding, hemopneumothorax.)


41 year old female who was stabbed through her right inframammary fold (aka under her right breast).
CT through 3 sequential phases shows a linear laceration through the right lobe of the liver. There is a small focus of contrast extravasation that enlarges over time, eventually spilling out of the liver into the peritoneal cavity. These findings are consistent with an AAST grade IV liver injury.
Oh, the knife also apparently went through the liver and diaphragm, into the chest cavity, because she also had a hemopneumothorax.
Her blood counts were trended and were stable, so she didn't need surgery for the liver laceration. She did have a chest tube placed for the pneumothorax.
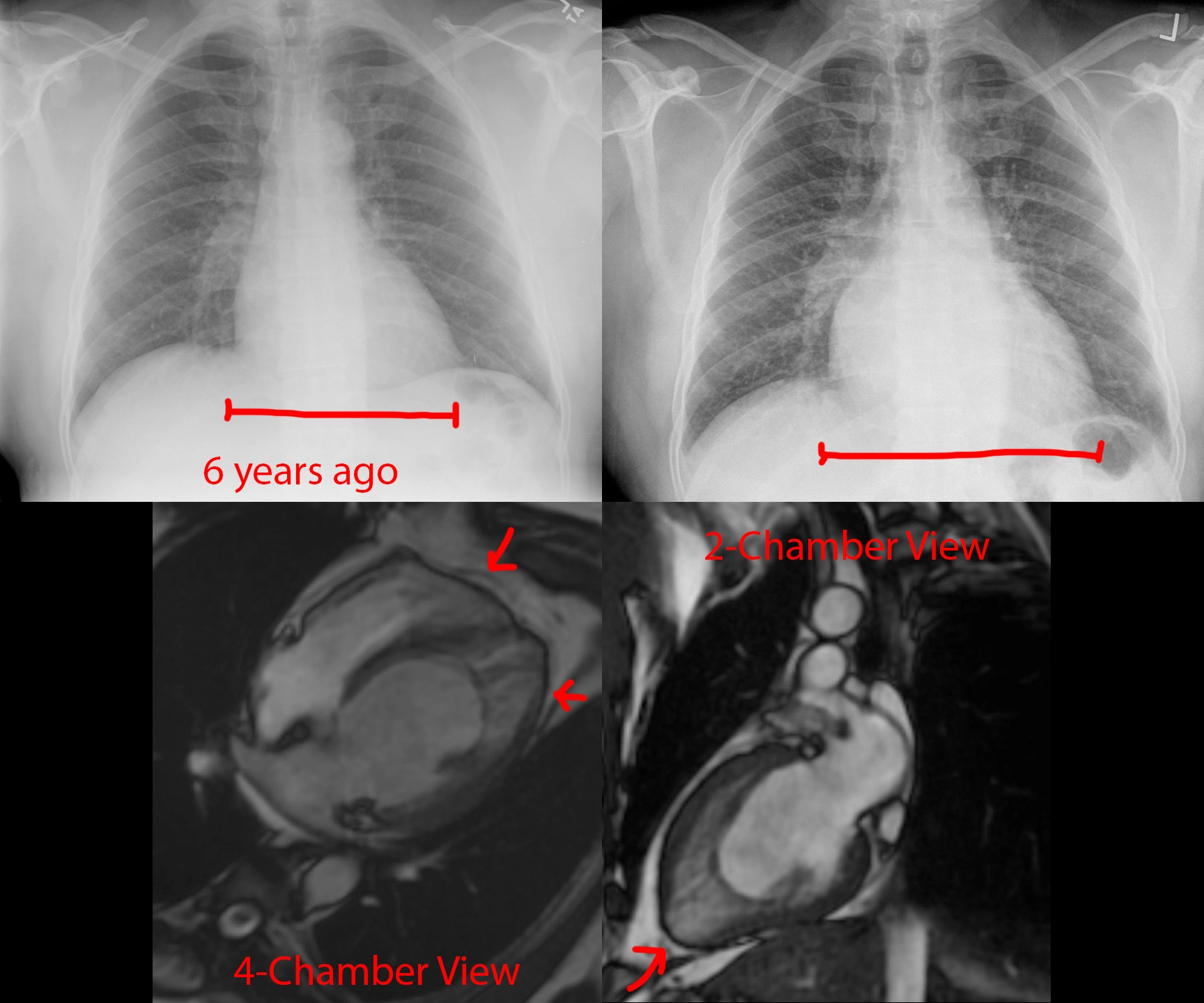
Pectus excavatum and its treatment.

12 year old with pectus deformity causing fatigue and chest pain. CT shows the really deep sternum indenting the heart. Cardiac echo (not shown) reported right ventricular compression to the point it was affecting systolic function. The patient had Nuss bars placed to correct the deformity.
Lethal left ventricular rupture.

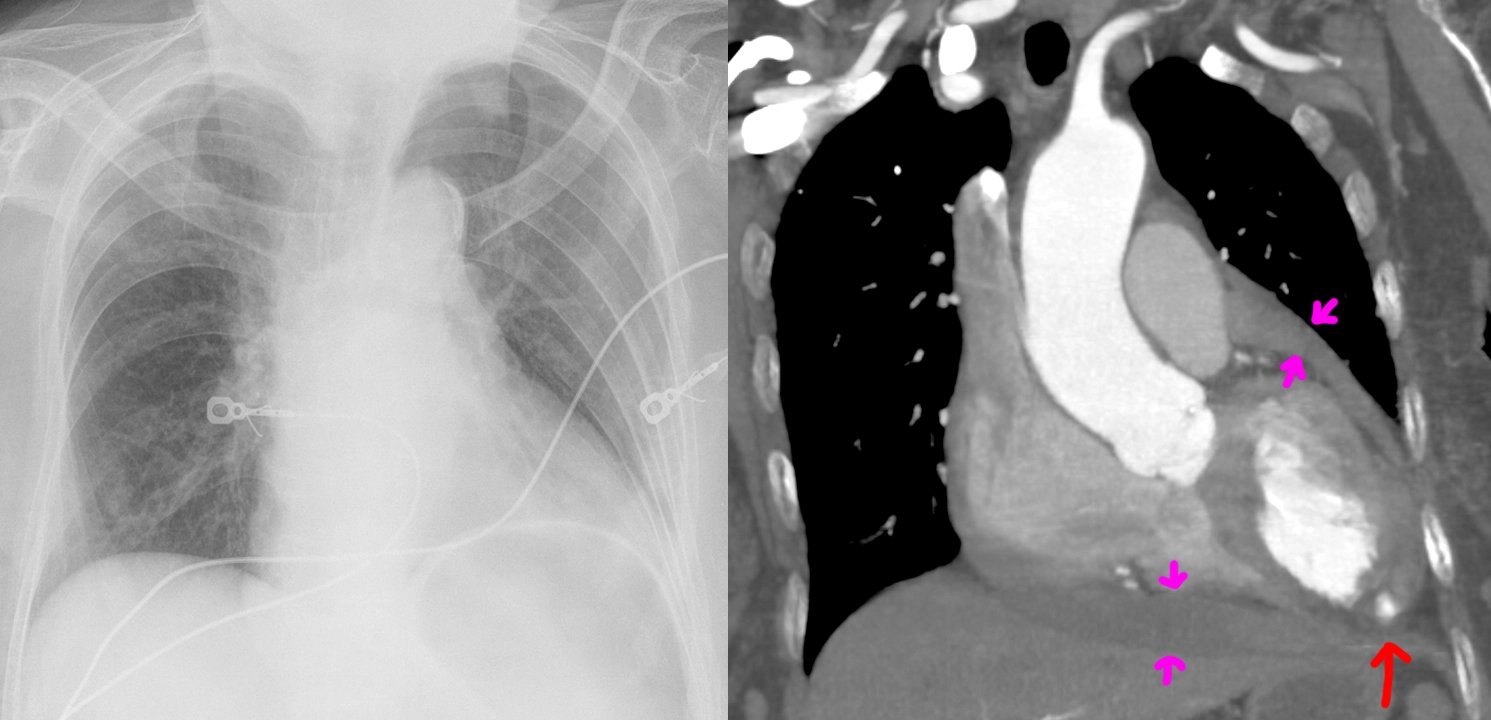
Elderly female with a history of hypertension, stroke, and, 1 month before, heart attack with cardiac arrest. The patient presented to the emergency department with 1 day of nausea, vomiting, cold sweats, and malaise. Troponins 1.54. ECG with inferior Q waves but no ST elevation/depression or T-wave inversion.
Chest radiograph shows an enlarged cardiac silhouette, for which a differential of cardiomegaly or pericardial effusion was suggested, as well as increased pulmonary vascular markings compatible with pulmonary congestion. Compared chest radiograph findings to the images from the methamphetamine-induced cardiomyopathy case.
CT angiography shows both cardiomegaly as well as an intermediate-density pericardial effusion (magenta arrows) concerning for hemopericardium. Most concerningly (holy-shit concerningly), there is a left ventricular aneurysm with rupture and blush of contrast (red arrow) into the hemopericardium, compatible with ongoing bleeding.
It is not surprising that a rupture of the heart carries high mortality risk. The patient passed away from PEA cardiac arrest shortly after admission, likely from cardiac tamponade by the enlarging hemopericardium.
Methamphetamine-induced cardiomyopathy.

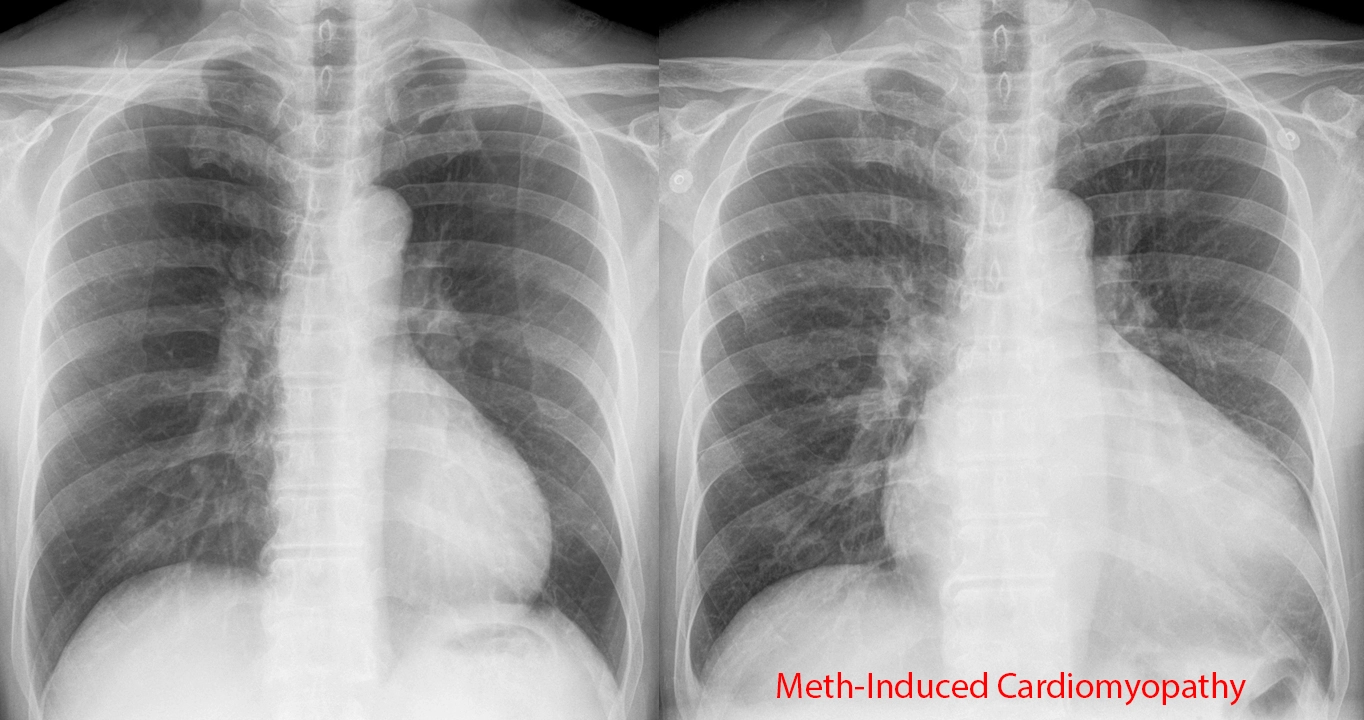
60 year old male with a history of homelessness, latent tuberculosis, and methamphetamine abuse. The patient was admitted to the hospital for shortness of breath and leg edema. A urine drug test on admission was positive for methamphetamine.
Chest radiograph (right) shows an enlarged cardiac silhouette, for which a differential of cardiomegaly or pericardial effusion was provided. Subsequent echocardiogram confirmed this was cardiomegaly with a low ejection fraction. The pulmonary vascular markings on the chest x-ray are also prominent, compatible with congestion from heart failure. The patient has a normal past chest radiograph (left) that provides an easy comparison for these findings.
A case of lung cancer and its cause.


I suppose it's fitting to start this community off with a case of one of the most common causes of morbidity and mortality in the world - smoking.
This patient presented to the emergency department for symptoms I no longer recall (probably shortness of breath or chest pain), which prompted a CT of the chest, whereupon the large spiculated mass in the right upper lobe was discovered. The lungs also demonstrate the typical findings for centrilobular emphysema. To my shame, I did not even notice the pack of cigarettes caught in the very same image at the time - it was the ED doc that noticed it when I called to notify about the lung mass.