Search
Grynfeltt-Lesshaft hernia. (This will be the last case I post for a few days.)

Incidental finding of a superior lumbar hernia (Grynfeltt-Lesshaft hernia). In this case, only a lobule of retroperitoneal fat is herniating through the defect, but organs can also herniate through.
Inguinal hernia containing bladder.
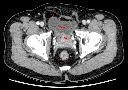
Continuing the theme of things extending into spaces they don't belong in, this is an incidental finding of an inguinal hernia that contains a small portion of the bladder. The patient got the CT for other reasons.
Bowel into inguinal hernia causing bowel obstruction.
Appendix into inguinal hernia, incidental finding.
Ventriculoperitoneal shunt into inguinal hernia, incidental finding.
Ovarian mucinous cystadenocarcinoma.
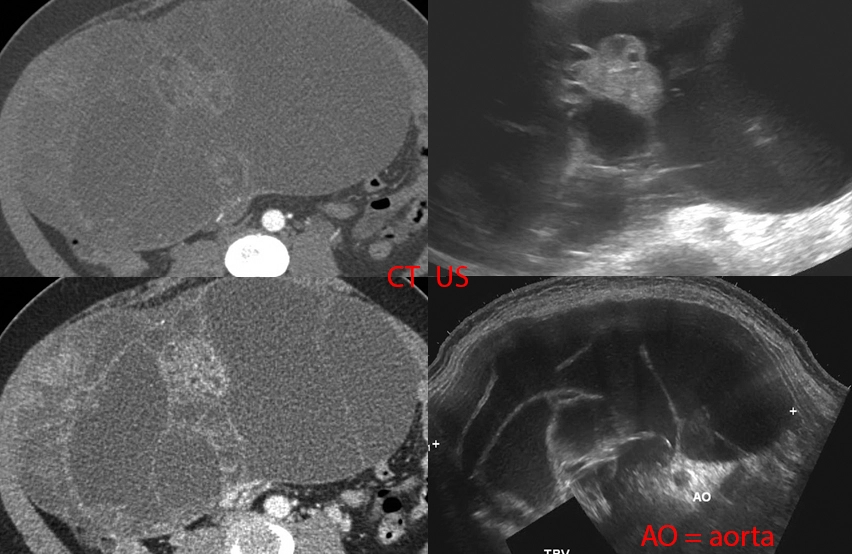
33 year old female with abdominal pain, abdominal distention, nausea/vomiting, early satiety, and weight loss.
Bottom right: Ultrasound done in a panorama shows how distended the abdomen is by a large multi-cystic mass.
Top right: Non-panoramic ultrasound image shows how limited the imaging modality is in being able to cover such a large mass. This image also shows a more solid area within the mass.
Left: CT images approximately where the ultrasound was done.
The patient underwent laparotomy with removal of the ovarian, fallopian tube, and appendix. There was a large ovarian cyst that was draining serous fluid (watery), mucinous fuid (mucus-like), and blood. The final path was as titled.
House, MD, pilot episode.

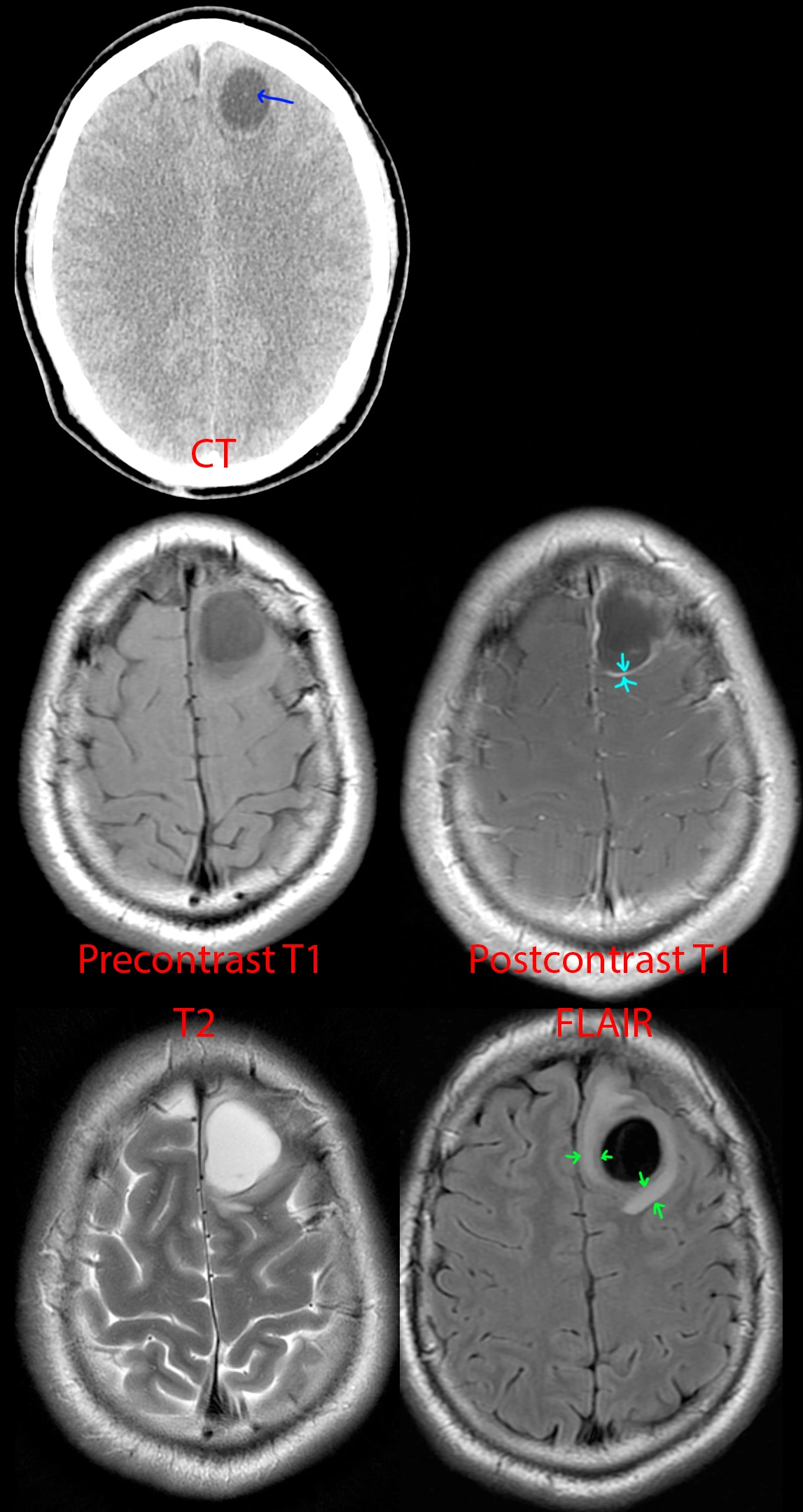
I remember this episode quite well because it happened around the time I decided to get into the medical field. In the episode, a young teacher had a first-time seizure while in the middle of teaching. House and team attempted to get a brain MRI, but she got an allergic reaction from the IV contrast. Thereafter, some drama happens, and at some point, they break into her house, find out she's been eating raw pork (wtf?), and diagnose her with the tapeworm infection associated with eating raw pork, cysticercosis (and neurocysticercosis, since it also involved her brain). They took an x-ray of her leg to show all the parasites in the muscles, and then House scolds her for being stupid. I remember thinking that was such as crazy medical story.
The reality is - they could have just repeated the brain MRI minus the contrast part, and the radiologist would have been able to identify neurocysticercosis without issue. House would have complained to Cuddy that she really was wasting his time with these basic cases, and the episode would have lasted 15 minutes tops...
Anyhow, this is a 25 year old Hispanic from jail. Just like the House episode, he presented with first time seizure and headaches.
CT of the head [top] shows a cystic lesion in the left frontal lobe. If one pays attention, one can see a small dot (blue arrow) within the cyst representing the scolex of the tapeworm parasite. Just from the CT appearance, history of seizure, and risk factors of jail (the parasite thrives in areas of low sanitation) and Hispanic (the parasite is endemic to South America), neurocysticercosis is the top possibility. A differential diagnosis of cystic brain tumor is provided to complete the picture.
MR [middle and bottom] shows a cystic lesion again. After giving IV contrast [middle right], one can see the cyst has a thin wall of enhancement (teal arrows). On T2 [bottom left] and especially FLAIR [bottom right], one can see a rim of swollen brain (green arrows) from the inflammation going on around the parasite.
This was diagnosed as neurocysticercosis in the colloidal vesicular stage and antiparasite medication was started.
23 year old with head injury since age 2. Seizures and right hemiparesis since age 10.
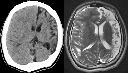
[Left]: Head CT shows left hemispheric volume loss. The injury happened early enough that even the skull is smaller on that side.
[Right]: Brain MRI shows the severe left hemispheric atrophy. Some of the brain gyri have bulbous ends and a thin neck, resembling mushrooms, a shape called ulegyria and consequence of the brain atrophy. The left lateral ventricle is mildly enlarged due to the atrophied brain.
Small bowel obstruction due to gallstone ileus.

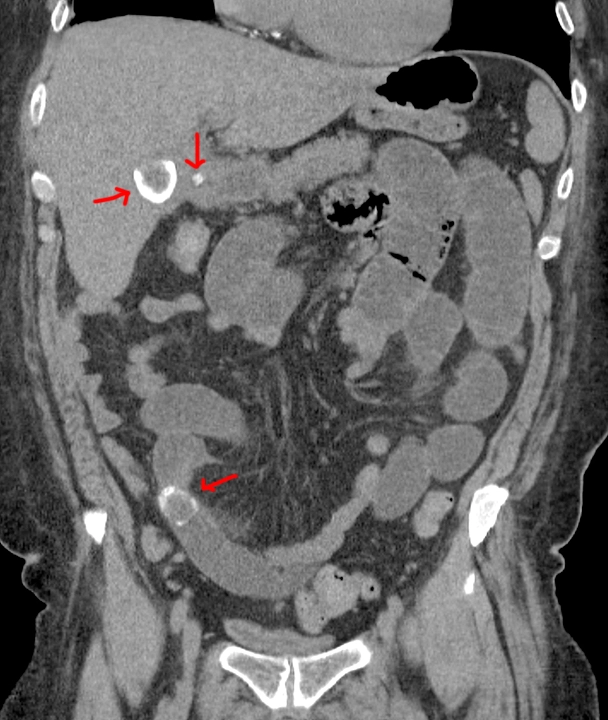
Red arrows point to 2 big gallstones, top one in the gallbladder and bottom one obstructing a small bowel loop, and a small gallstone in the cystic duct.
Small bowel obstruction from incarcerated inguinal hernia.


Red lines point to hernia entry. Red arrow points to where the bowel tapers and becomes obstructed as it enters the hernia sac.
Crohn's disease.

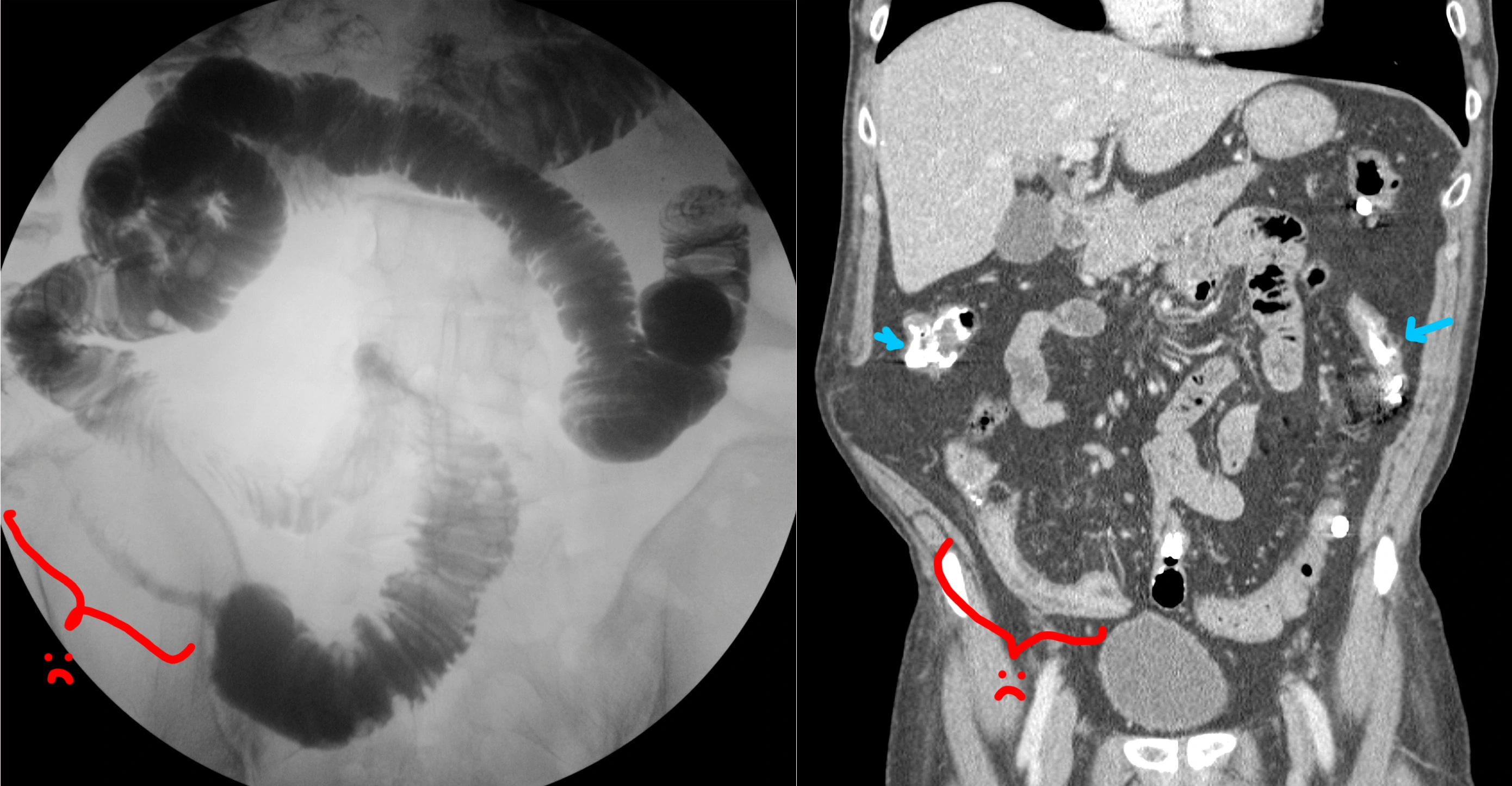
No clinical history saved on this one - sorry.
[Right] Small bowel follow-through (SBFT), where the patient drinks barium, and then we wait a bit until that barium is in the small bowel, then we take some pictures. This study is showing a long segment of terminal ileum that is strictured and severely narrowed in fibrostenotic Crohn's (red bracket). This is called the "string sign."
[Left] Coronal CT performed sometime after the SBFT. You can still see some residual barium in the small and large bowels (blue arrows). Red bracket shows the CT appearance of the terminal ileum stricture. On the CT, you can also see that the strictured segment has submucosal fat deposition, the "fat halo sign."
Two patients showing the varied appearance of large B-cell lymphoma of the stomach.

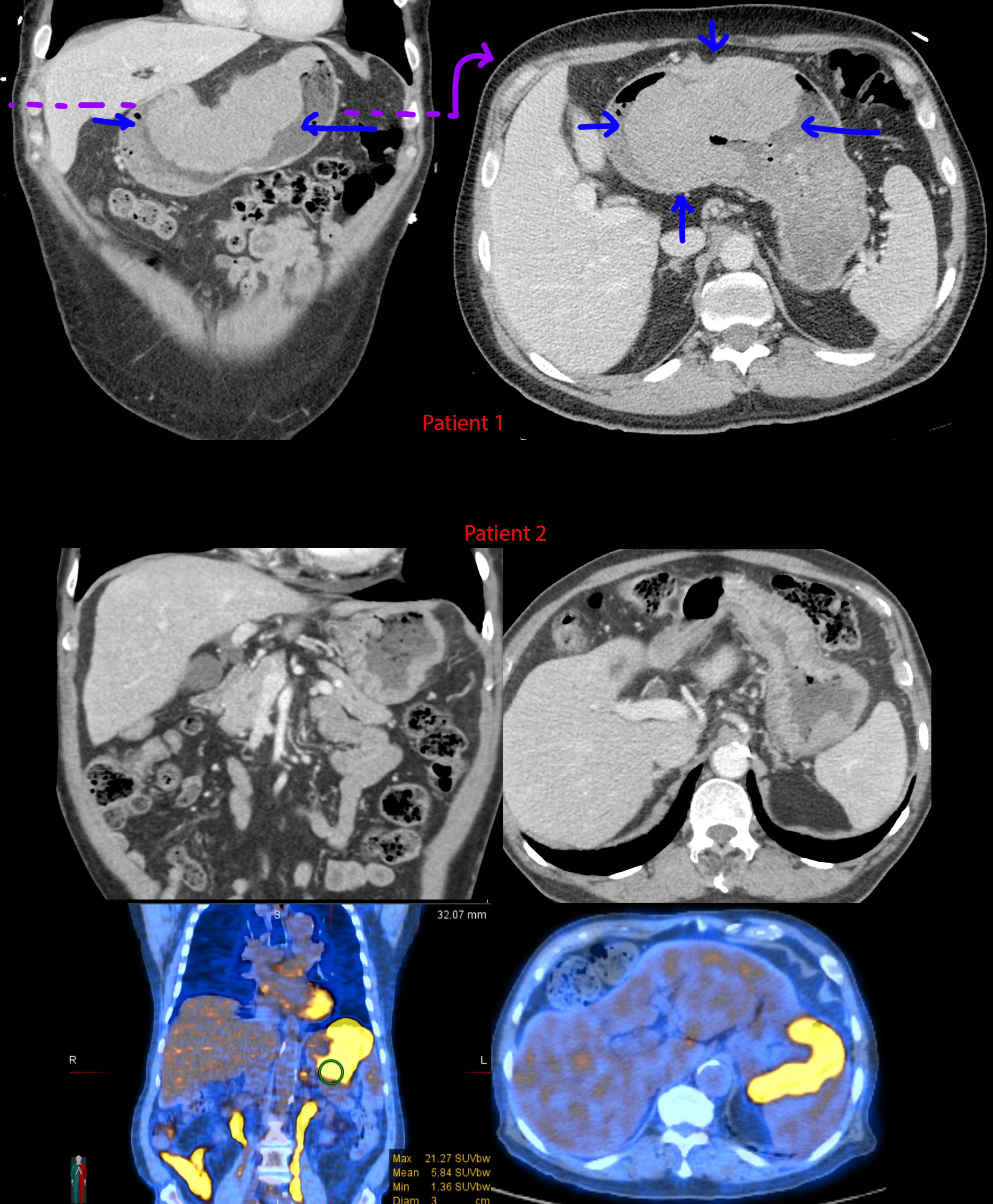
I didn't save any clinical history for these - sorry.
[Top] Patient 1 - Gigantic mass along the lesser curvature of the stomach. Look down at your belly - this mass is about 1/3rd the width from left to right.
[Mid] Patient 2 - CTs showing gently lobulated and undulating wall thickening of the gastric cardiac and fundus. Notice the transition from the normal gastric rugae to the smoother wall thickening where it is infiltrated by lymphoma. There is also mild (aneurysmal) dilation of the stomach where the wall thickening is located.
[Bottom] Patient 2 - PET-CT. The wall thickening is ridiculously hypermetabolic with a max SUV of 21.3. For comparison, the liver is normally in the range of 2-4 mean SUV.
Tuberculosis, sarcoidosis, lymphoma, and metastatic disease - these 4 can look like almost anything.
Left kidney stone.

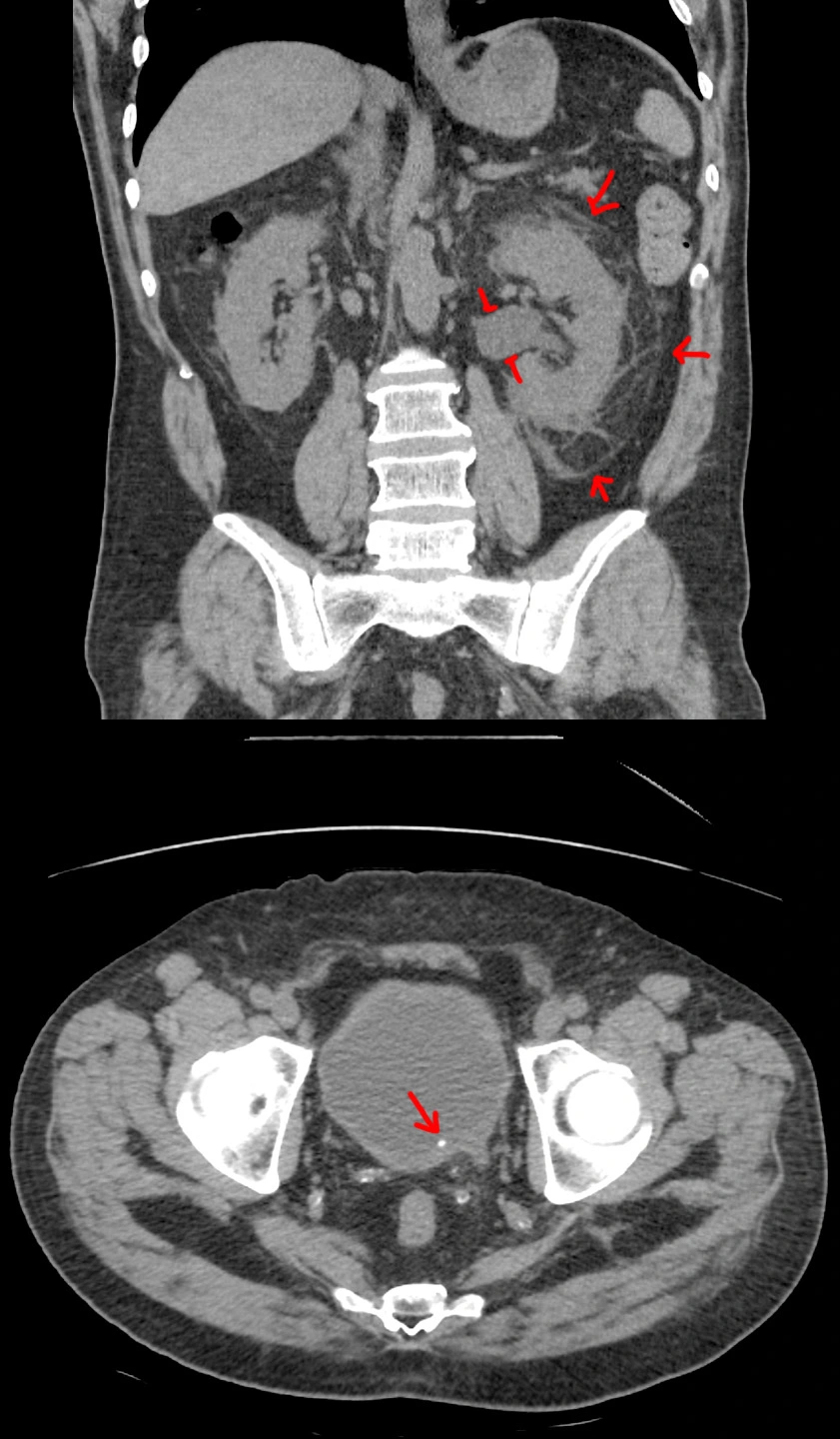
57 year old with left flank pain for 12 hours. Urine sample 2+ for blood. White count at 14.
[Top]: Coronal CT shows the left kidney is enlarged, with angry-looking, inflamed, surrounding fat. The renal pelvis is dilated (hydronephrosis).
[Bottom]: Axial CT shows a small stone at the very end of the ureter (ureterovesicular junction).
Pretty straightforward case. For the nonmedical visitors, this is what we look for if your doc wants to get a CT for flank pain / kidney stone suspicion. See the other case for an ultrasound version.
12-ft fall with loss of hearing.

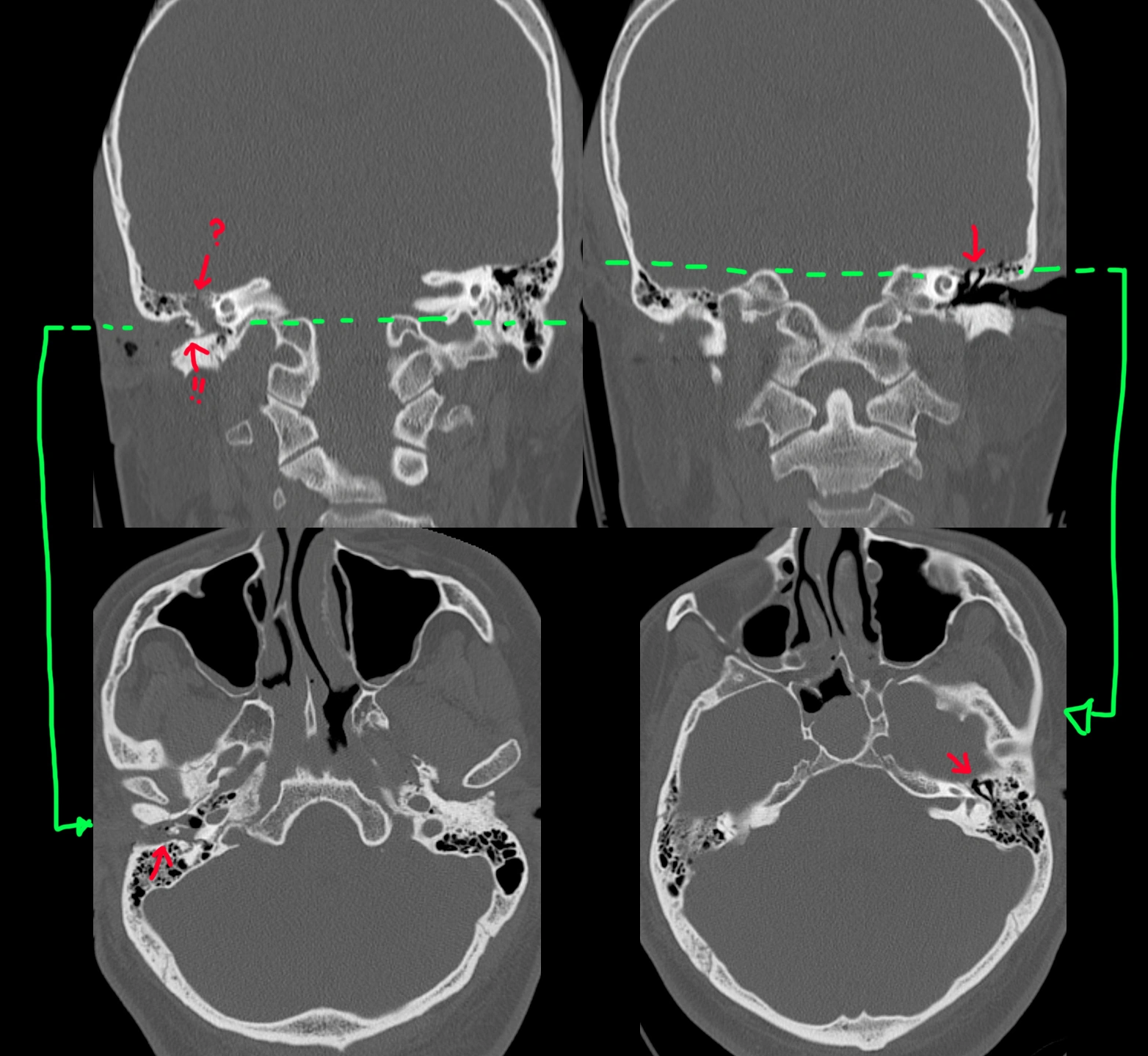
31 year old doing some doing roof work when he fell. Seen in the ED with right ear bleeding and right-sided decreased hearing.
The normal left side is depicted in the right images (standard convention). Coronal view [top right] shows the middle ear ossicles (arrow) in the middle ear cavity, and axial view [bottom right] shows the normal "ice cream cone" appearance (arrow).
By comparison, the right middle ear ossicles are missing in the middle ear cavity [top left] (arrow with ?) and found in the external auditory canal (arrow with !!) instead. Axial view [bottom left] shows a distinct lack of the ice cream cone appearance. The middle ear and external ear canals are also filled with fluid/blood. The tympanic membrane is clearly ruptured since the middle ear ossicles are outside.
Abdominal distention despite being told her uterine fibroids "shrunk" after menopause.

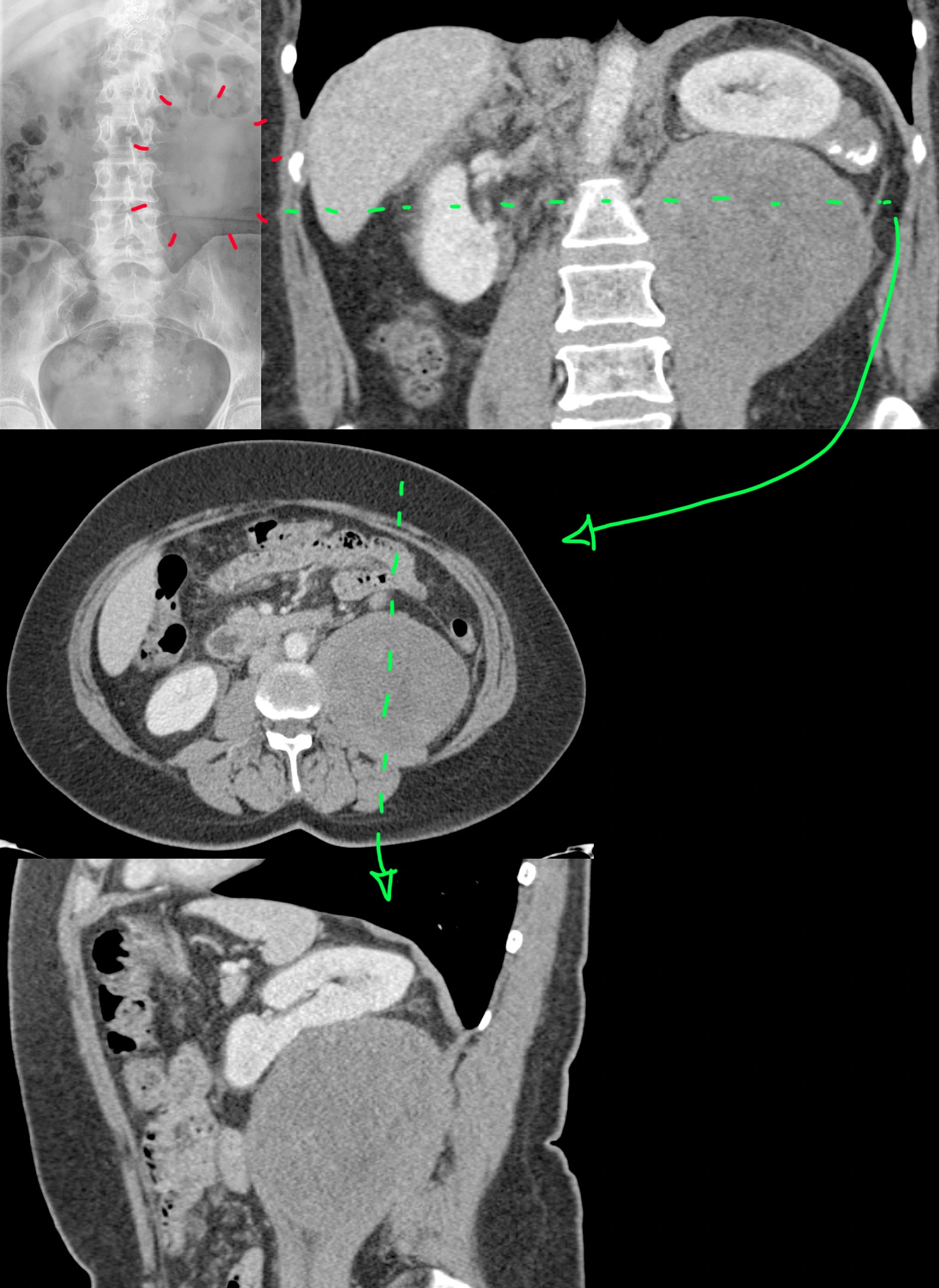
54 year old female with a history of uterine fibroids with persistent abdominal distention despite being told her fibroids shrunk after menopause - presumably via some pelvic ultrasound, which we didn't have.
Abdominal X-ray [top left] was possibly was called normal, which is not completely unreasonable. However, with the help of the follow-up coronal CT [top right], one can see that there is a vague area lacking any bowel gas that looks like it could be a mass. Axial [middle] and sagittal [bottom] CTs show a nonspecific, solid mass, well-circumscribed, with no calcifications, cysts, hemorrhage, or fat inside. The left kidney is pushed up by the mass, but the fat plane between the two is preserved with no evidence of renal invasion.
The patient underwent surgical resection.
Final diagnosis: Retroperitoneal dedifferentiated liposarcoma.
Tuberculous pancreatitis and lymphadenitis.
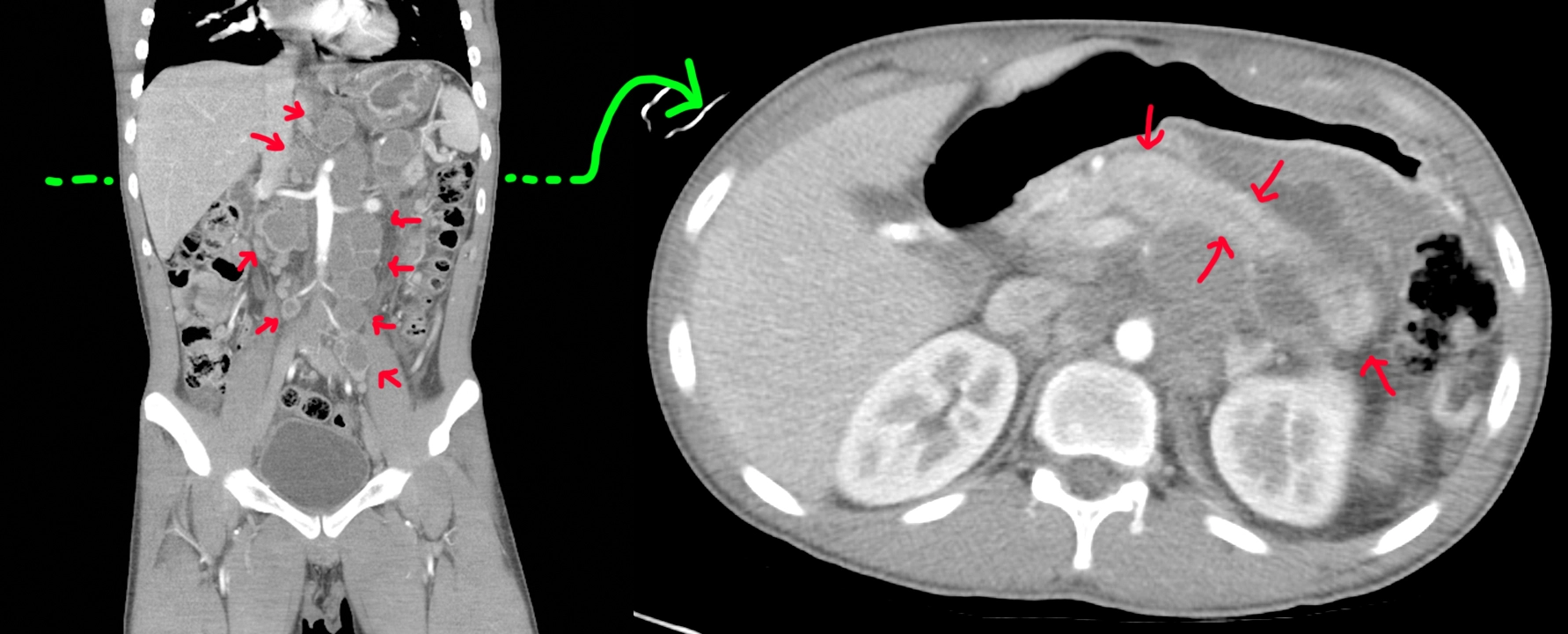
20 year old with a history of trisomy 21 and recent travel to Vietnam. Was seen there for nausea, vomiting, and abdominal pain with diagnosis of acute pancreatitis and what looked like lymphoma (but negative biopsy).
Coronal CT [left]: Big retroperitoneal lymph nodes with central cystic change/necrosis (red arrows).
Axial CT [right]: Done at the level of the green line shows a sausage-shaped pancreas compatible with ongoing versus resolving pancreatitis (red arrows).
Repeat EGD/EUS with celiac lymph node biopsy shows caseating granulomatous inflammation with positive culture and PCR for tuberculosis.
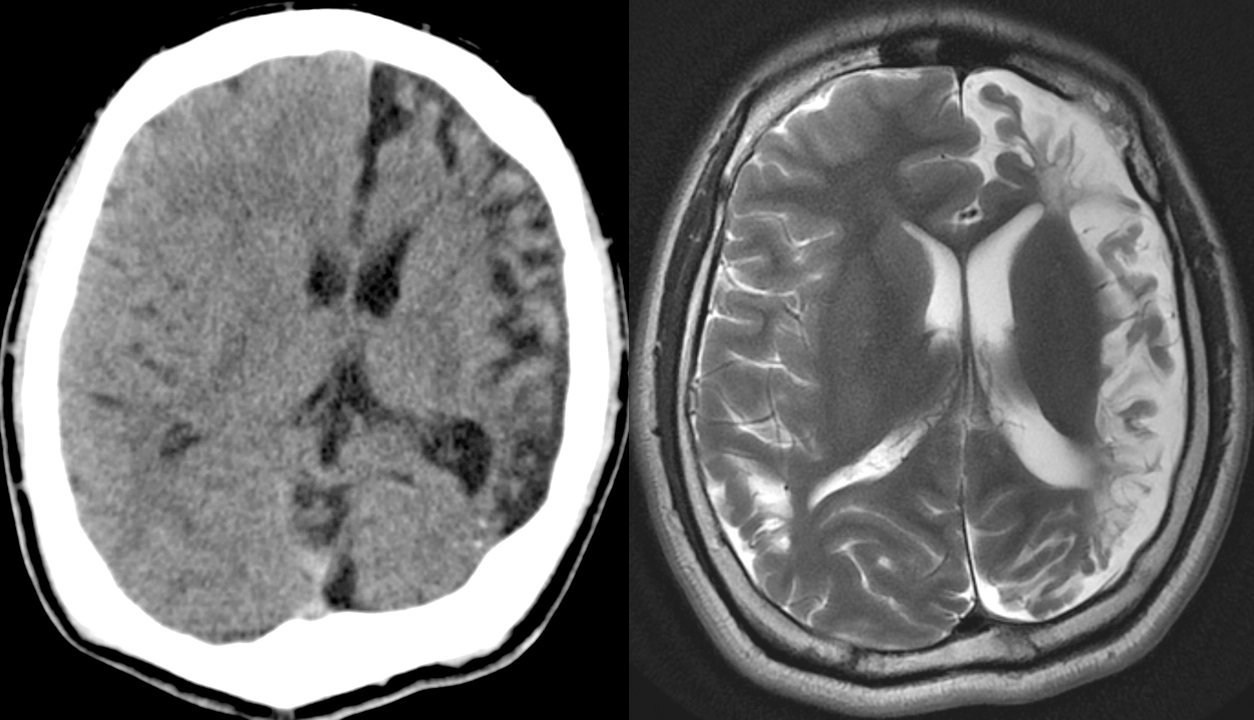
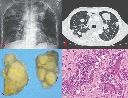
Patient with HIV-AIDS, tapeworm infection, and new fever, cough, fatigue, and weight loss.
This is an absolutely insane case that made the NEJM rounds a couple years ago now. I wish this was mine. I don't think there's been another case report like it since.
41 year old Colombian male with HIV-AIDS (not adherent to treatment), tapeworm infection, with several months of fever, cough, fatigue, and weight loss.
Top left: Chest x-ray shows multiple round lung masses.
Top right: Chest CT shows those round lung masses. Look like metastases.
Bottom left: The tumors taken out.
Bottom right: Pathology of the tumors.
The patient underwent empiric treatment for tapeworm and HIV with progression of masses. The CDC was contacted for help when treatment wasn't working.
The tumor cells clearly looked like cancer but were too small to be human cells. Genetic sequencing ultimately showed tapeworm DNA, with mutations and genetic rearrangements compatible with cancer.
Final diagnosis: Metastatic tapeworm cancer, likely developed because the patient had no immune system from the HIV-AIDS.
The patient passed away a few days after the diagnosis was finally made.
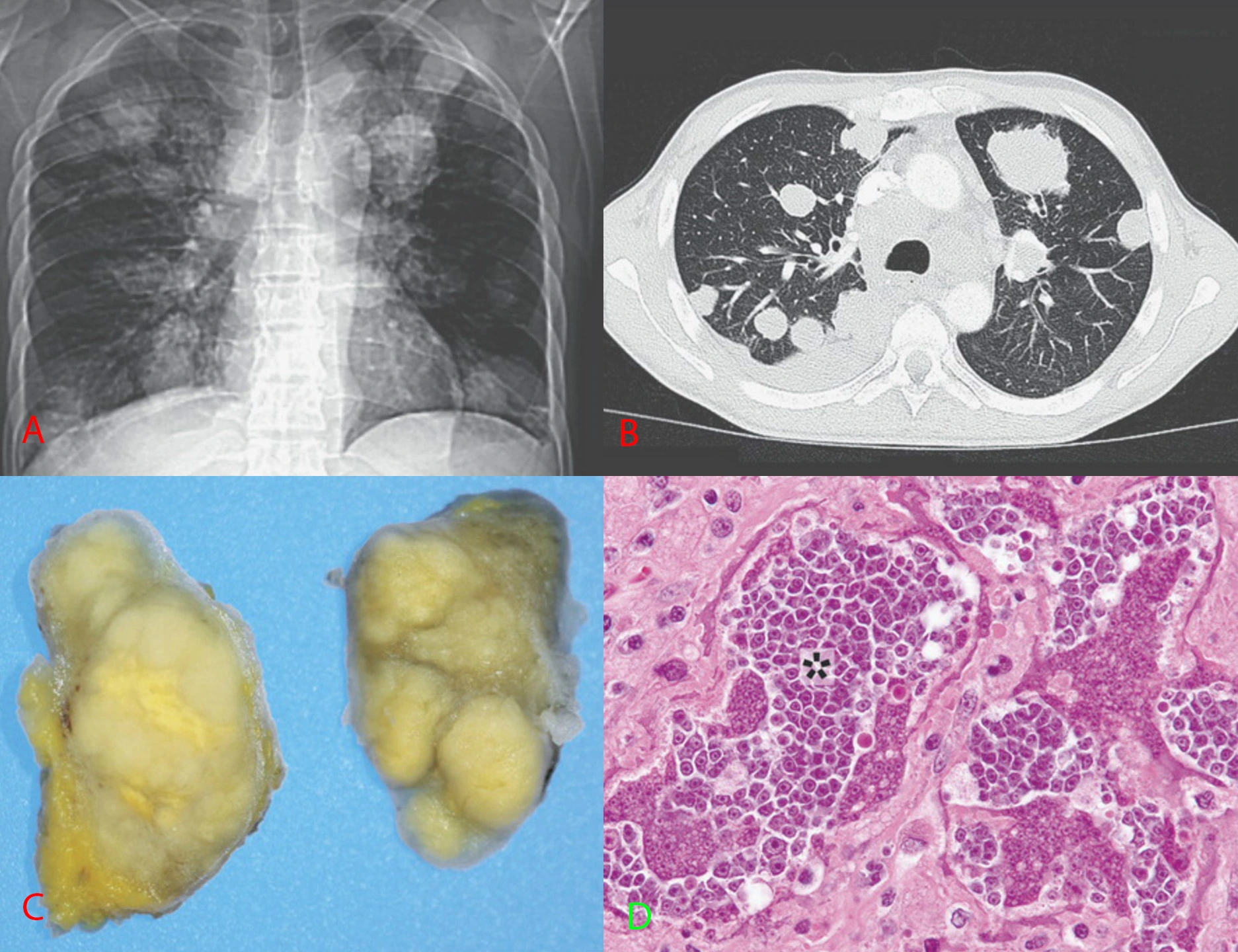
52 year old who keeps getting pneumothoraces.
52 year old with a remote history of a rare skin cancer, dermatofibrosarcoma protuberans (DFSP) now presenting with recurrent pneumothoraces and difficulty breathing.
Top: Frontal and lateral chest radiographs shows the lungs filled by numerous cysts of varying sizes. Some cysts have layering fluid in them forming fluid levels.
Bottom: Axial CT through the mid lungs shows the numerous cysts, some with layering fluid, some with wall thickening.
Differential diagnosis for cystic lung disease: airway disease (emphysema, bronchiectasis from various causes), infectious/inflammatory (abscesses, vasculitis), cellular proliferation (cystic metastases, papillomatosis, mesenchymal cystic hamartomas, eosinophilic granulomas, lymphangioleiomyomatosis), injury (traumatic cysts, old lung infarcts).
Final diagnosis: The history of a histiocytic skin cancer suggested an extremely rare entity for cystic lung disease called pulmonary cystic fibrohistiocytic tumor.
It is sort of unclear if the lung cysts represent metastases from the fibrous histiocytic skin cancer or a separate primary neoplasm. The disease has an indolent progressive course. There is no good treatment for this as far as I am aware. These patients also get pulmonary arteriovenous malformations that might need embolization - you can see this patient does have a few embo coils on the chest radiographs at the left lung base.
"Crazy coworker stabbed her at her house." (Liver laceration with active bleeding, hemopneumothorax.)


41 year old female who was stabbed through her right inframammary fold (aka under her right breast).
CT through 3 sequential phases shows a linear laceration through the right lobe of the liver. There is a small focus of contrast extravasation that enlarges over time, eventually spilling out of the liver into the peritoneal cavity. These findings are consistent with an AAST grade IV liver injury.
Oh, the knife also apparently went through the liver and diaphragm, into the chest cavity, because she also had a hemopneumothorax.
Her blood counts were trended and were stable, so she didn't need surgery for the liver laceration. She did have a chest tube placed for the pneumothorax.
Bilateral indirect inguinal hernias. Appendix enters right inguinal hernia (Amyand hernia).

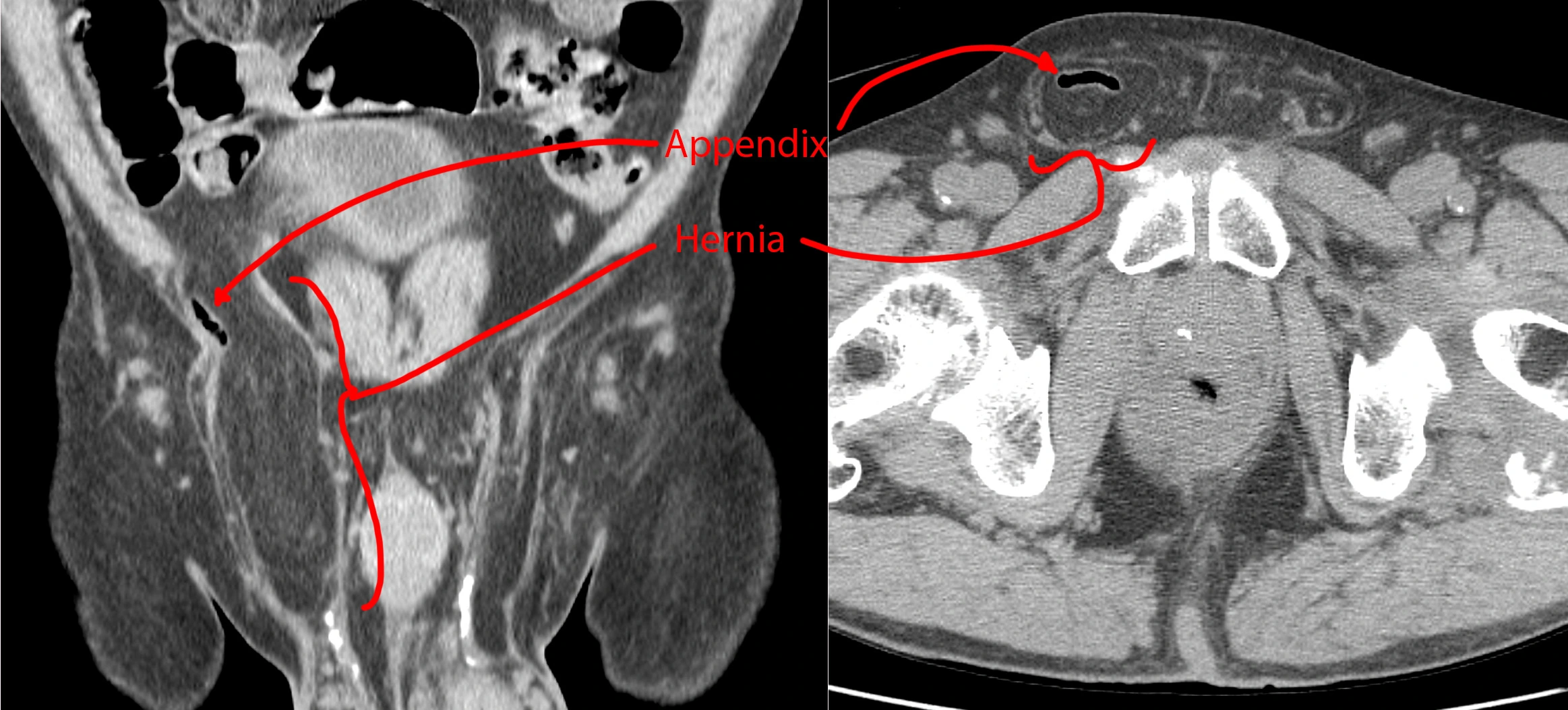
A companion case to this one. Bilateral groins with fat-containing hernias. The right-sided hernia also has a small air-filled tubular structure consistent with an appendix. There are no inflammatory changes to suggest acute appendicitis, so this is an incidental finding.
A right inguinal hernia containing an appendix is called an Amyand hernia and apparently pretty rare at <1% of inguinal hernias.
Bilateral indirect inguinal hernias. Ventriculoperitoneal shunt terminates in right inguinal hernia.

45 year old with a ventriculoperitoneal shunt (VPS) for history of toxoplasmosis. Incidental finding - no symptoms.
CT shows bilateral groin fluid collections. The right fluid collection contains the distal loops and tip of the VPS. So, just an incidental bit of cerebrospinal fluid in the groin.
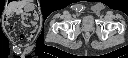
Endometriosis.

36 year old female with a history of C-section. Then she started feeling a growing mass in her surgical scar.
CT shows a spiculated mass along the C-section scar that invades the right inferior rectus muscle. A differential diagnosis of desmoid tumor, endometriosis, and soft tissue sarcoma was provided.
Surgical resection of the mass was performed, which turned out to be endometriosis.
Gnathic (jaw) osteosarcoma.

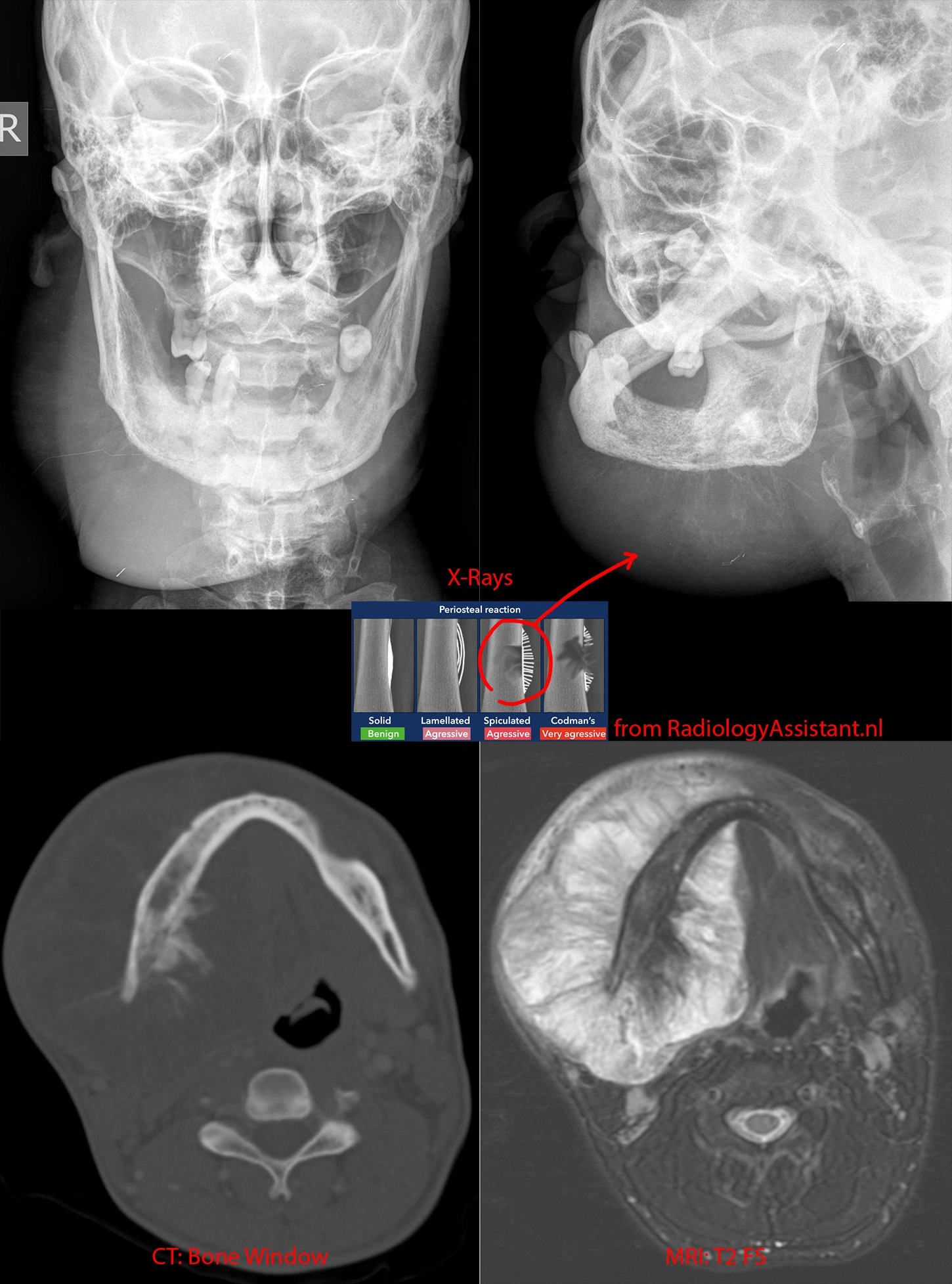
Top left and right: X-rays showing a BIG right jaw mass. Whispy calcifications likely represent spiculated periosteal reaction, a very aggressive bony reaction.
Bottom left: CT in the bone/calcification window shows the periosteal reaction better.
Bottom right: MR in the T2 sequence shows the full extent of the jaw mass and how it extends far beyond the mandible's margins, both outward and inward into the floor of mouth.
While this mass is very large, in general, jaw osteosarcoma has a better prognosis than conventional osteosarcomas.